Taking Cost Containment Further Left: From Prepay to Pre-Claim Provider Education
Create a More Positive Provider Experience While Eliminating Denials, Appeals, and Resubmissions by Ensuring Claims Accuracy Before Submissions.
Codoxo Launches Point Zero Payment Integrity
Shifting Left Is No Longer Optional
Let us help you
intervene earlier
act more proactively
protect your provider relationships
protect your bottom line
Helping Healthcare Organizations Like You Break the Status Quo
Proudly reducing healthcare costs for over 80 million lives and trusted by top healthcare payers, government agencies, and pharmacy benefit managers (PBMs)
Taking Payment Integrity Further Left Than Anyone in the Industry – Pre-Claim Provider Education Changes Everything
Our platform provides critical insights directly to providers, enabling them to submit claims accurately the first time and avoid the entire cycle of denials, appeals, and resubmissions that damages payer-provider relationships.
By addressing issues before claims are even created, we eliminate the downstream abrasive payment integrity activities that frustrate providers and create administrative burden – all within a single generative AI-driven Unified Cost Containment Platform.
Our unified platform delivers:
- Pre-Claim Provider Education: Deliver insights before claims are created, ensuring first-submission accuracy
- Elimination of Abrasive PI Activities: Avoid denials, appeals, and resubmissions entirely
- Stronger Provider Relationships: Transform adversarial interactions into collaborative partnerships
- Comprehensive Coverage: Seamlessly integrate pre-claim, prepay, and postpay solutions in one platform
- Superior ROI: Achieve $60+ PMPY in cost savings with less provider friction
We’re on a mission to make healthcare more affordable and effective for everyone.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
Codoxo’s Unified Cost Containment Platform leverages generative AI and advanced automation to shift left in the payment cycle, enabling earlier intervention, proactive cost avoidance, and stronger provider relationships—all within a single, unified platform.
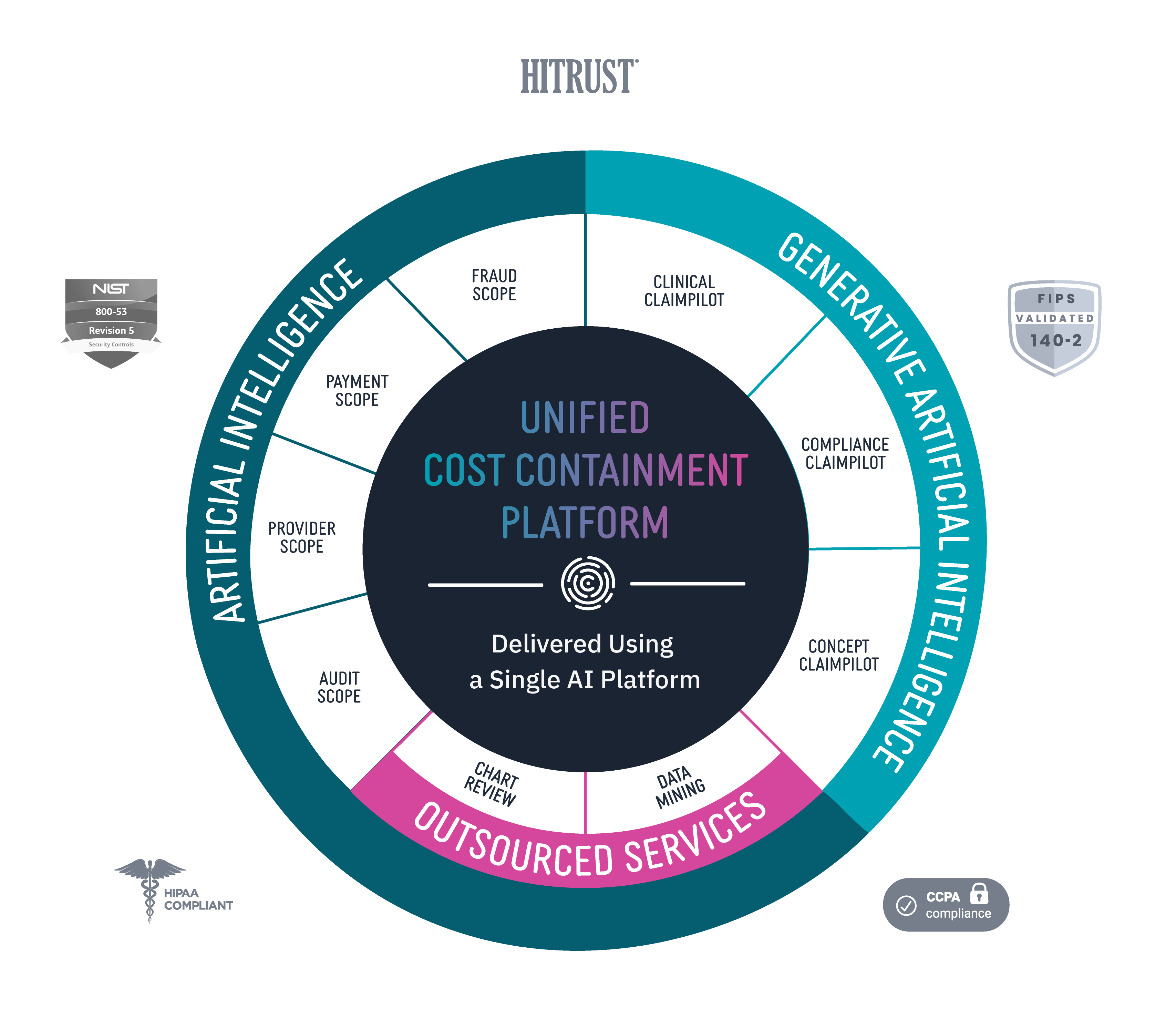
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
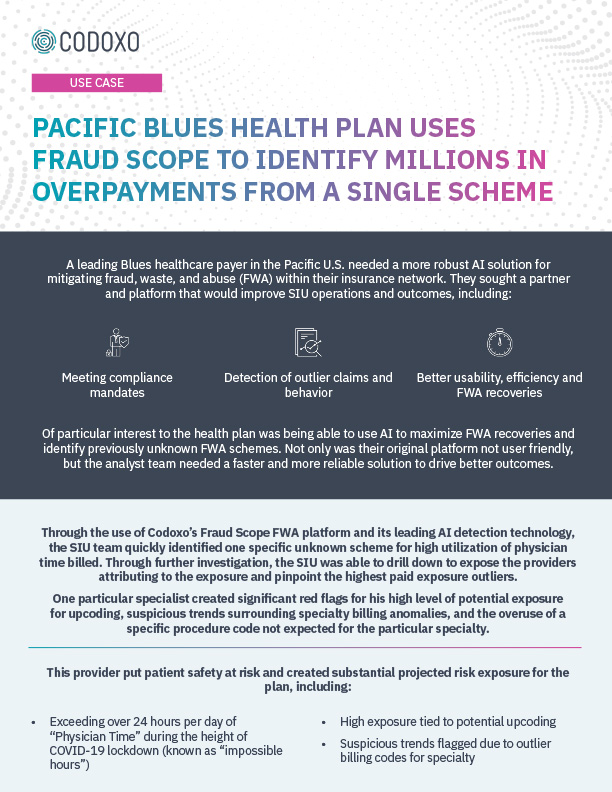
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.
Move Payment Integrity Programs Upstream.
Generative AI-Driven Unified Cost Containment Platform
Powered by advanced generative AI and self-learning AI, Codoxo unites teams into a single platform for faster, earlier – and more accurate payment integrity. Covering all critical areas—provider education and network services, payment integrity, and Special Investigation Units (SIU) — it seamlessly integrates prepayment and postpayment processes, enabling more efficient and effective cost management.
By focusing on the earliest intervention and education, healthcare payers foster stronger relationships with providers through early provider education, resolving potential issues before claims are submitted.
Healthcare Cost Containment Results
$60+ PMPY
in cost savings throughout your entire cost containment journey
700% increase
95% faster
policy loading with 50% greater accuracy
10x
more efficient emerging threats identification
90% gains
in workflow automation and productivity
99% reduction
in payment errors, improving accuracy and reducing manual intervention
20x to 30x
Eliminates
40% reduction
in overpayments