Maximize Recoveries With
AI-Powered Healthcare Fraud, Waste, & Abuse Detection & Prevention
Ready to Unlock 3X ROI With Fraud Scope?
Fraud Scope
Fraud Scope empowers SIU teams with AI tools to detect and prevent fraud, waste, and abuse (FWA) faster and more accurately than ever. By analyzing claims in real time, and through proprietary AI technology, it enables rapid and accurate identification of outlier claims and providers, uncovering hidden patterns for early intervention. Fraud Scope streamlines time-consuming tasks like provider communication, medical record reviews, and claims analytics to enhance investigator efficiency and precision.

Empower Your SIU with Advanced AI & Gen AI-Driven FWA Solutions for Unmatched Accuracy & Maximized Recoveries
Fraud Scope equips healthcare payer, PBM and agency SIU teams and investigators with the tools to uncover more actionable leads for recovery.
Industry-leading & patented healthcare artificial intelligence
The fastest and most accurate fraud, waste, and abuse detection
Streamline investigations workflow & evidence tracking
Consolidated case management details within one customizable platform
Generative AI-powered medical record reviews
Expedite investigations by automating time-consuming, manual record reviews
Combines AI, rules & advanced analytics
Detect outliers across all claim types, all codes, and all lines of business including Medicare fraud, Medicaid Fraud, and Commercial fraud, as well as medical, dental, and prescription fraud
Customizable, user-friendly reporting tools
Easily share insights and reports to meet SIU targets, compliance needs, and SIU goals
Save time & uncover more outlier behavior
Effortless query development empowers teams to act faster and drive more impactful investigations
Reduce setup time from months to weeks
Accelerate
SIU workflows
Elevate Your Healthcare Fraud Detection With Codoxo’s Proprietary Self-Learning AI
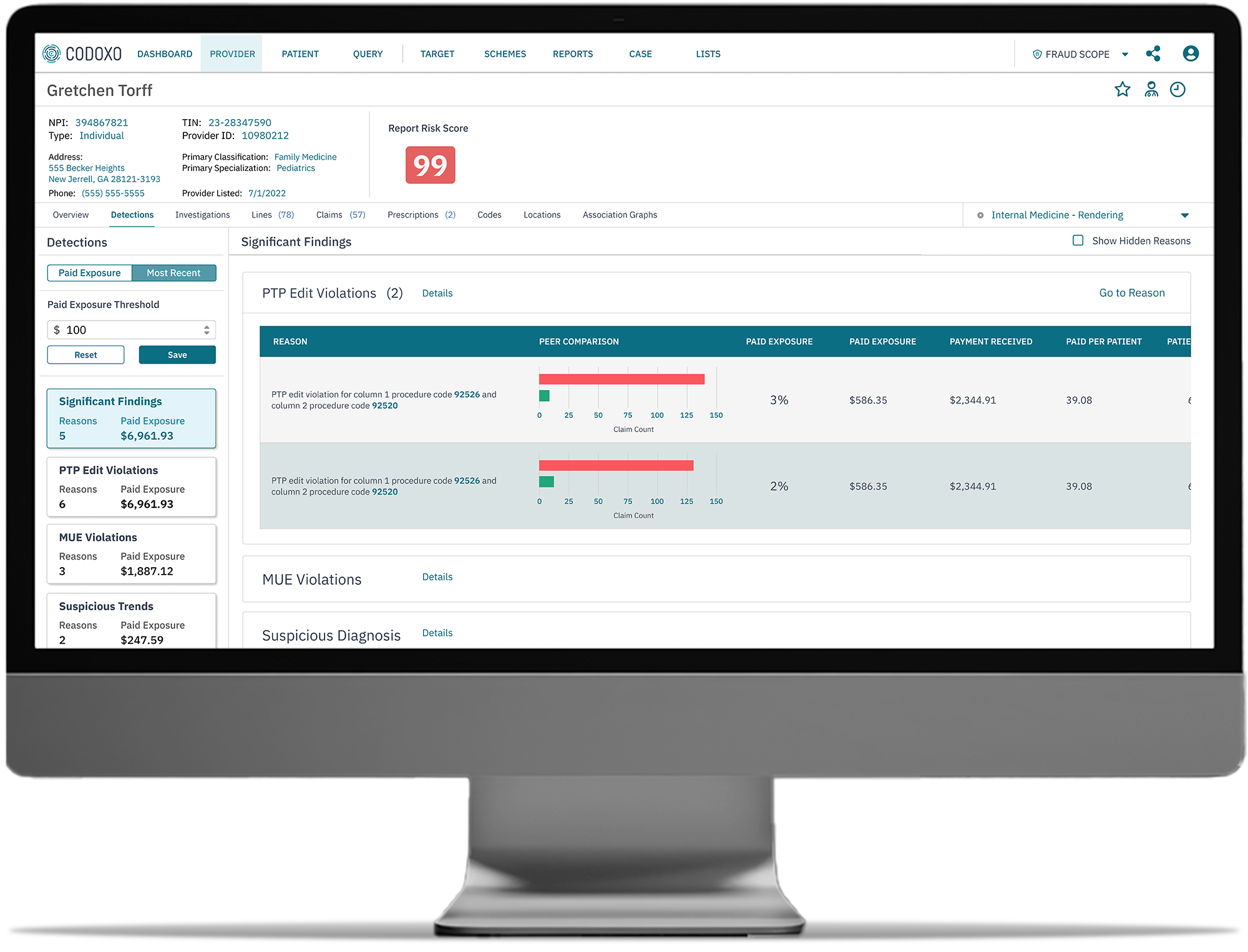
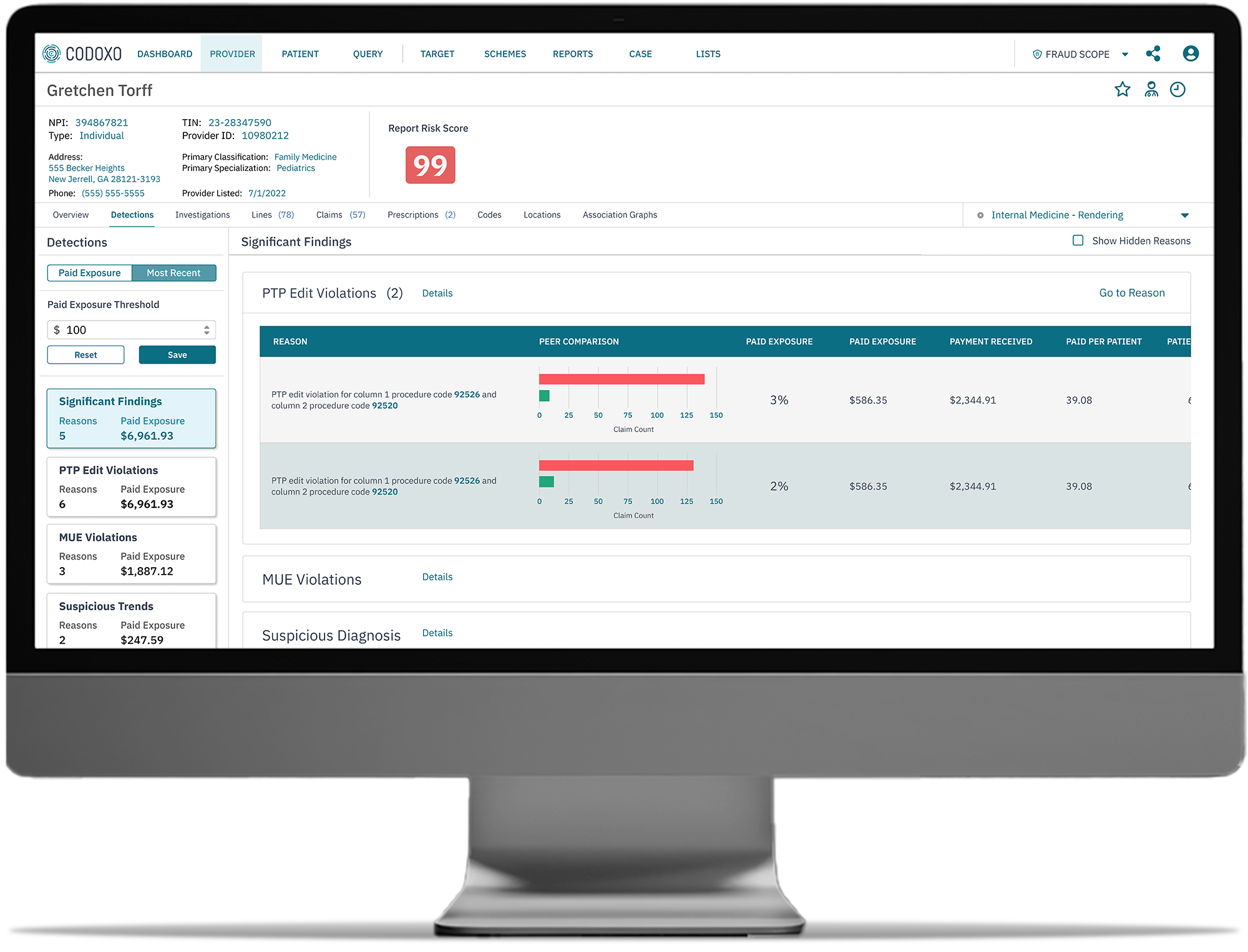
- Clear evidence chains
Automatically gathers evidence chains and presents them clearly for external compliance reporting, with the ability to deep dive in order to validate findings - Prioritization of suspicious claims
Use the Codoxo Claims Risk Score and dollar amounts to prioritize review and investigation - New risk alerts & active watchlists
Flag claims from providers, facilities, pharmacies, or other practices suspected of fraud, waste, and abuse for easier tracking - Provider integrity score
Measures the potential for fraud, waste, and abuse using a proprietary system that analyzes data to detect anomalies in user behavior consistent with fraudulent activity - Built-in generative AI-powered natural language query tool
Simplifies data exploration and enables rapid query creation
- User-friendly interface
SIU users can quickly and easily access and understand fraud schemes through an intuitive interface, querying functionality, and clear scheme explanations - Geo analytics & mapping
Identifies the relationship between members and providers grouped by area - Provider engagement views
Permission-controlled holistic view of engagement with providers across SIU, Payment Integrity, and Provider Education - Customizable reports & insights
Create easy-to-interpret custom reports to meet stringent and evolving compliance and regulatory requirements - Accelerate data exploration
Built in generative AI-powered natural language query tool with a user-friendly interface for intuitive querying and clear scheme explanations
The Fraud Scope Advantage
100%
$30M
$25M
$6M+
Smarter Healthcare Cost Containment Starts With Codoxo
Fraud Scope is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI and generative AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
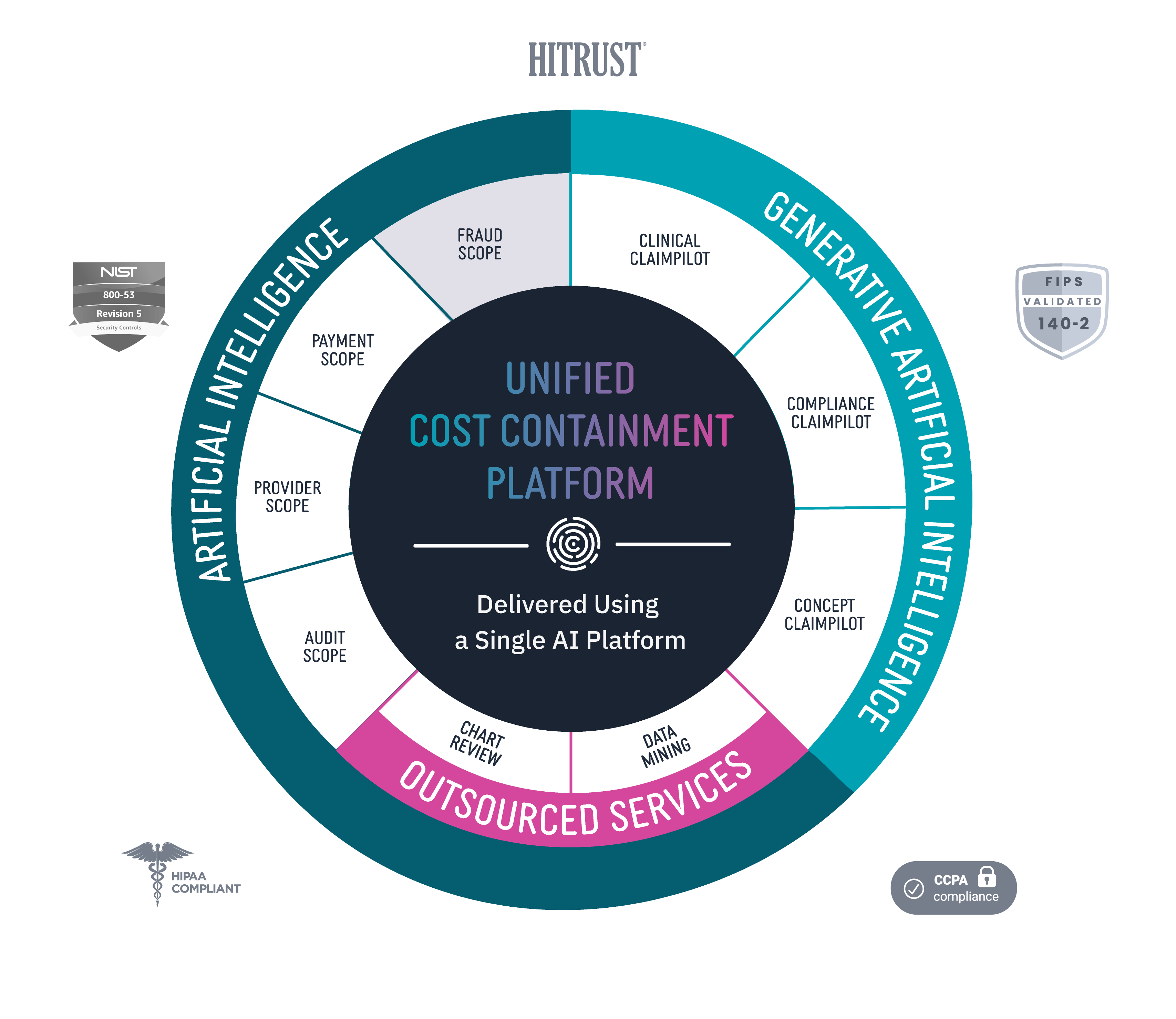
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.