Save Costs & Ensure Claims Accuracy Prepayment with
AI-Powered Analysis


Achieve 99% Error Reduction for Improved Healthcare Payment Accuracy.
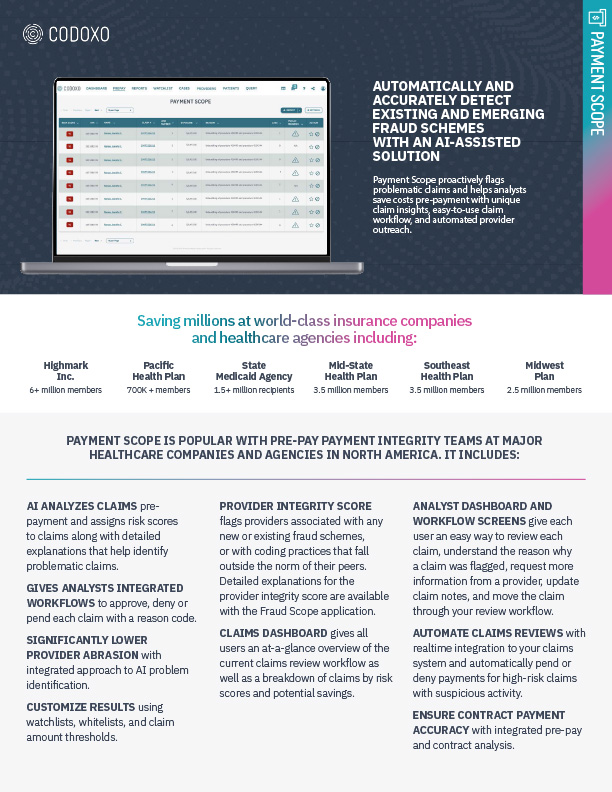
Payment Scope
Help your team identify emerging issues and outlier behaviors more quickly, efficiently, and accurately than traditional methods.

Empower Your Bottom Line with a Single Cost-Saving Solution
Leverage industry-leading AI
To quickly and accurately detect problematic claims and emerging issues
Empower payment integrity teams
With an all-in-one platform with streamlined workflows for claim reviews
Handle more claims prepay
By quickly analyzing claims data and assigning risk scores for faster decision-making
Easily share insights & reports across departments
To meet payment integrity goals, compliance mandates, and cost containment targets with customizable, user-friendly tools
Reduce provider
abrasion
With proactive monitoring and automated workflows, minimizing unnecessary provider interactions
Ensure contract payment accuracy
By integrating prepay and contract analysis to ensure payments align with contract terms
Automate & Enhance Payment Integrity With Advanced AI-Driven Technology
- Provider integrity score
Detailed analysis of provider behavior to identify anomalies in coding practices and detect potential fraud based on peer comparisons - User-friendly interface & insights
At-a-glance overview of claims review workflows, including risk scores and cost efficiencies, for streamlined monitoring - Easy-to-interpret reports & insights
Pre-built and customizable reports designed to meet stringent and evolving compliance and regulatory requirements - Customizable results
Custom results using watchlists, whitelists, and claim amount thresholds to provide tailored insights, supporting payment integrity and healthcare claims accuracy
- Automated claims review
Real-time integration with claims data for automated review,
pended payments, or denial of high-risk claims and suspicious activities - Risk alerts & active watchlists
Automated alerts and watchlists for tracking providers, facilities, or other entities at higher risk for claim accuracy issues - Analyst dashboard & workflow screens
Centralized interface for claim review, provider communications, and workflow management, enhancing user efficiency
Boost Healthcare Payment Accuracy with Payment Scope
99%
Prevents
improper payments before they happen
Improves
Enhances
Smarter Healthcare Cost Containment Starts With Codoxo
Payment Scope is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI and generative AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform Products & Services
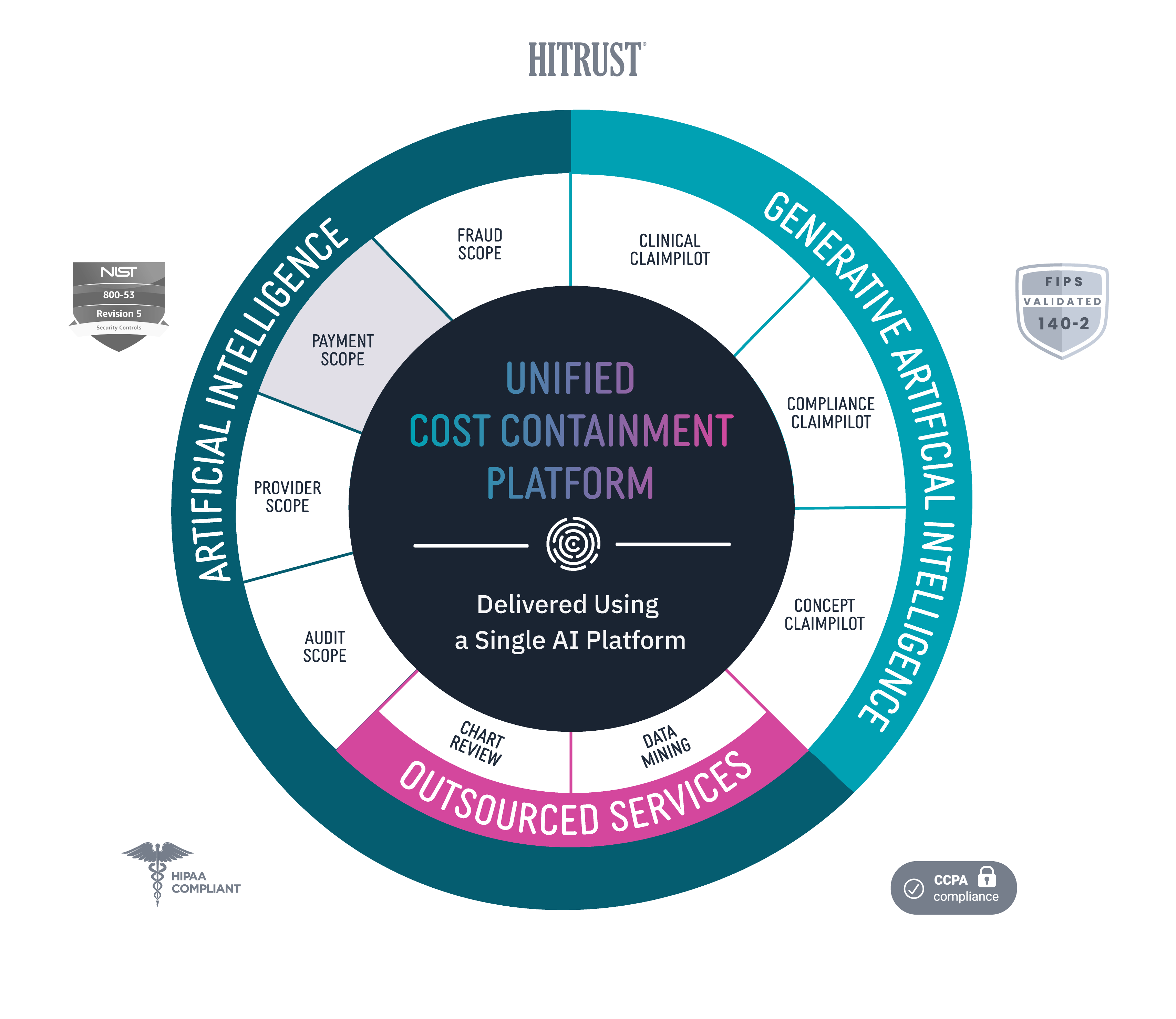
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.