Adhere to Provider Reimbursement Policies With More Accurate Payments & Better Provider Experience
Harness the power of generative AI to strengthen provider relationships through enhanced payment accuracy, with faster medical policy reviews and provider contract compliance.
Achieve 95% Faster Policy Loading Time.
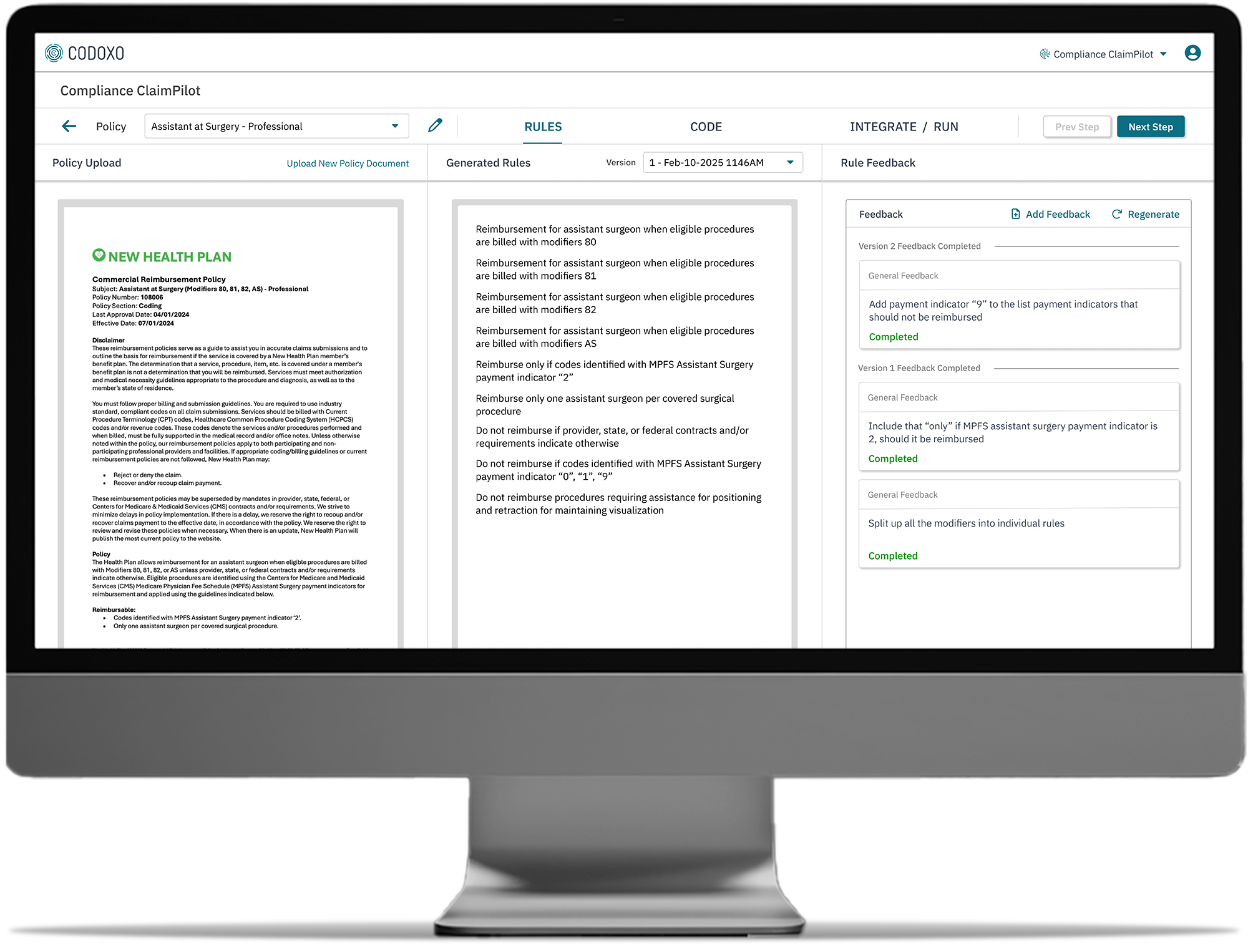
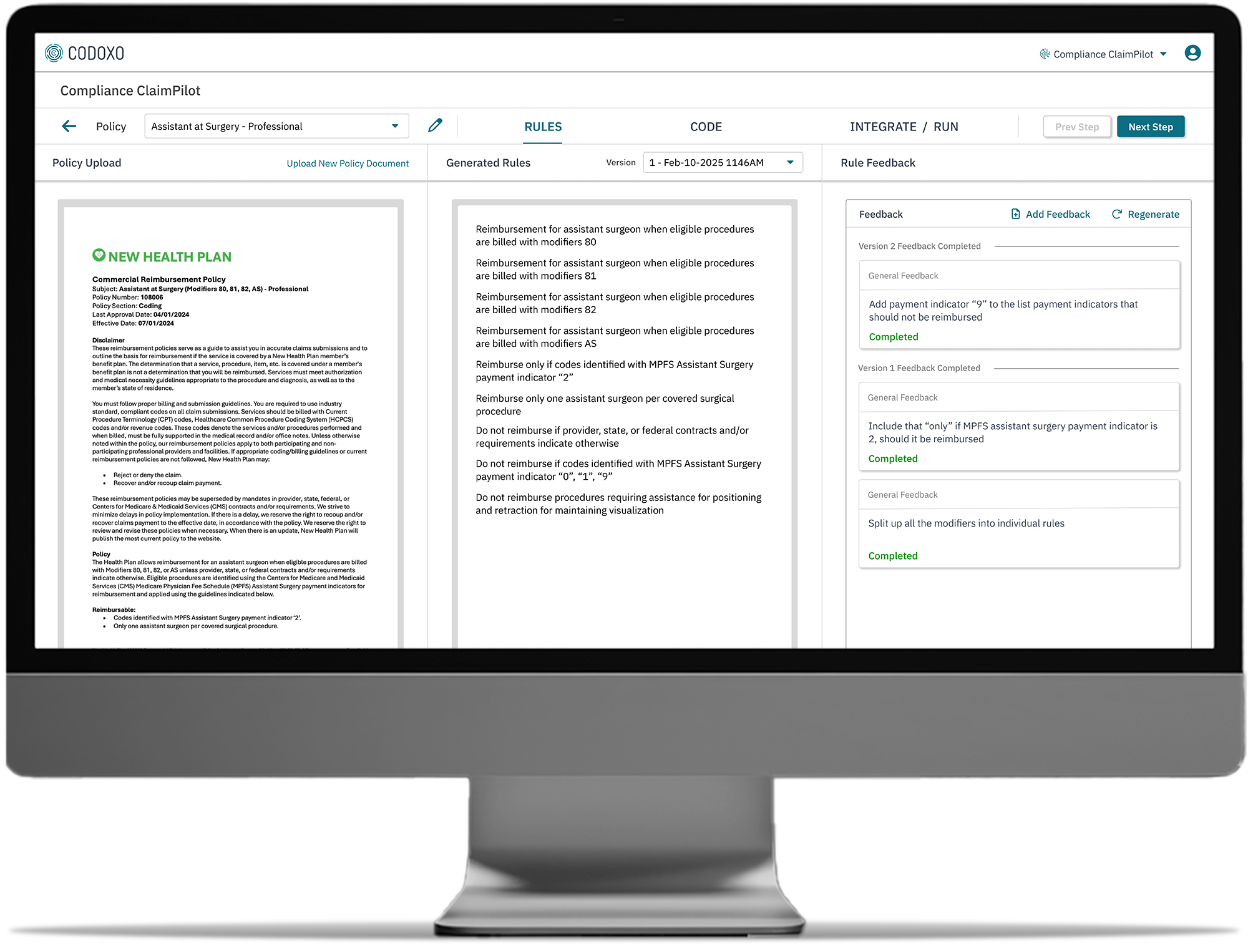
Compliance ClaimPilot
Compliance ClaimPilot automates the process of creating rules based on provider reimbursement policies and applying them for claim review. Automation paired with broader rules coverage, early error detection, and up to 99% reduction in incorrect claim payments, Compliance ClaimPilot sets new benchmarks for provider experience, cost savings, compliance monitoring, and efficiency.
Compliance ClaimPilot is part of Codoxo’s ClaimPilot suite of Generative AI-driven payment integrity solutions, including:

Transform Adherence to Provider Contracts Through Generative AI-Driven Automation
Reduce incorrect claim payments
Fostering stronger provider relationships and minimizing financial risks
Reduce costly errors & improve processing speed
Using generative AI to scan reimbursement policies and provider contracts to ensure accurate claim payments
Enhance visibility into policy enforcement & provider contract terms
Improving compliance monitoring and payment integrity with clear, user-friendly formats
Earlier detection & correction of claims errors
Mitigating financial risks and ensuring accurate reimbursements
Enables broader rules coverage
Automating the process of creating rules based on provider reimbursement policies and applying them for claim review
Streamlines compliance management
By leveraging generative AI to automate the validation of adherence to reimbursement policies and contract requirements during medical policy reviews
Outperform Traditional Solutions with Generative AI-Powered Provider Contract Compliance Monitoring
- Accelerated processing
Significantly reduce the time to validate adherence to reimbursement policies and contracts - Intuitive compliance monitoring
Simplify complex contract terms and medical policies for non-experts
- Real-time insights
Detect and correct inaccurately processed claims early, improving billing outcomes and claims accuracy - Provider-friendly
Foster smoother relationships by resolving billing discrepancies faster
Setting New Payment Integrity Standards
95%
faster application of reimbursement policy during claims review
faster contract loading
Smarter Healthcare Cost Containment Starts With Codoxo
Compliance ClaimPilot is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform Products & Services
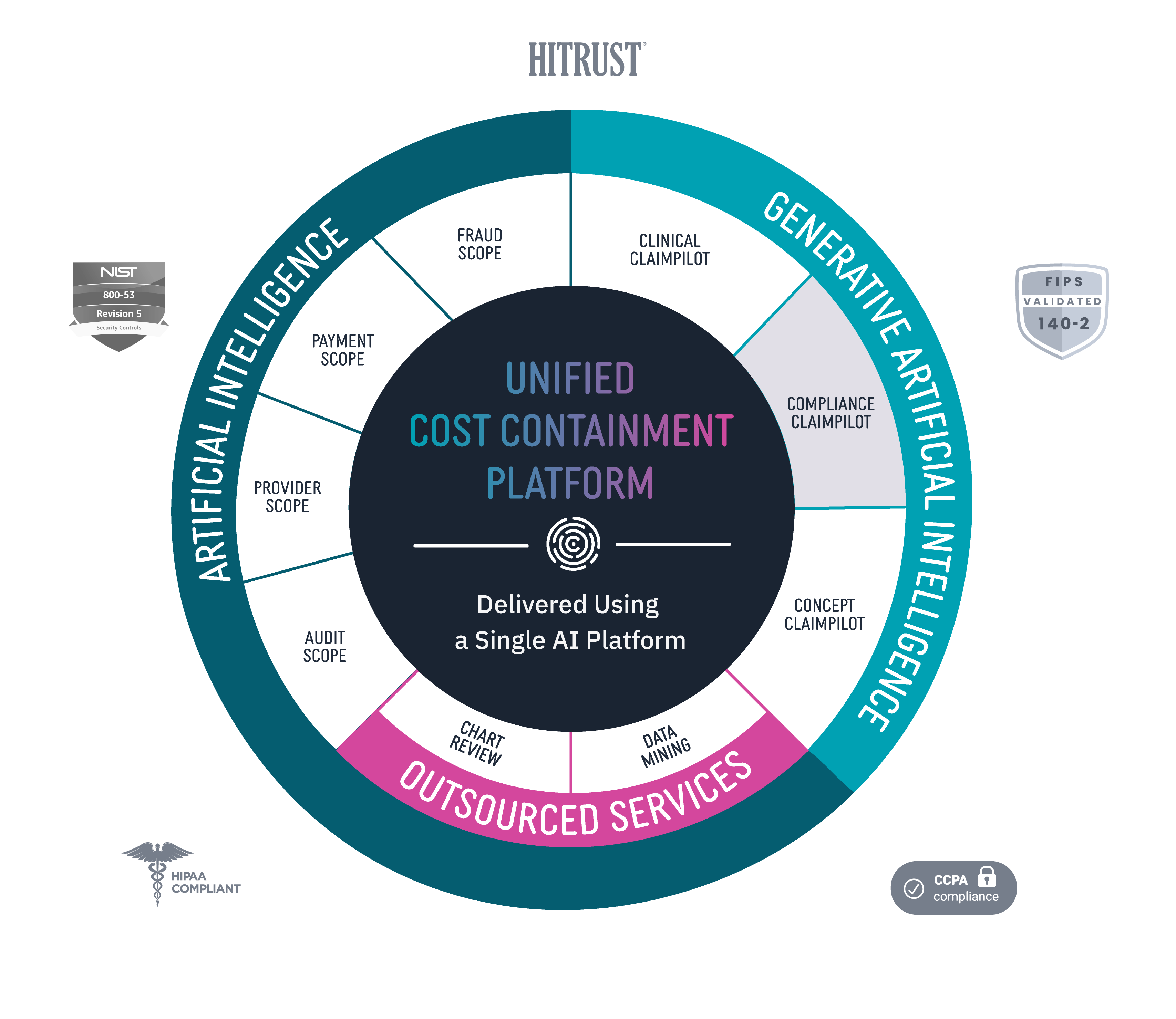
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.