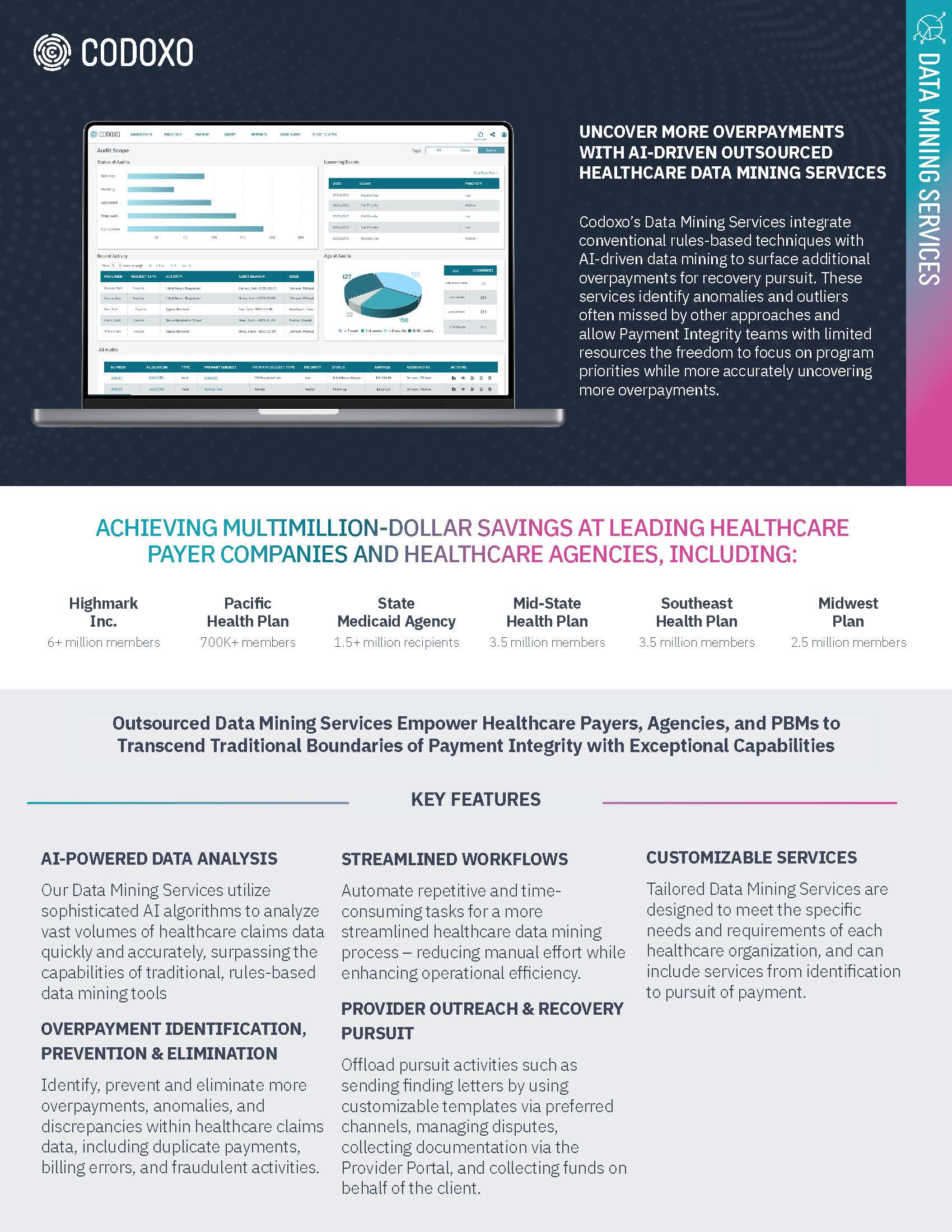
Data Mining Services
Uncover More Overpayments & Increase Recoveries with AI-Driven Healthcare Data Mining Services
Codoxo’s Data Mining Services help uncover additional overpayments for recovery with precision and efficiency. Leveraging advanced AI tools, our payment integrity experts identify anomalies and outliers often overlooked by other solutions.

Ready to Realize $5 PMPY on Your Data Mining Efforts?
Codoxo’s Data Mining Services combine cutting-edge AI with expert analysis to uncover missed overpayments, detect anomalies, and flag waste, abuse and errors in billing and payment. Offering flexible service options, Codoxo can manage some or all aspects of the data mining process — ranging from initial identification to provider outreach and recovery efforts — tailored to meet each client’s unique needs for seamless and efficient results.
Empower your payment integrity team with maximized recoveries while reducing manual workloads.
Maximizing Overpayment Detection & Recovery with AI-Powered Data Mining Services
Healthcare payment integrity teams face increasing pressure to detect overpayments, abuse, waste, and billing errors while managing resource constraints. Offloading data mining to Codoxo allows these teams to leverage advanced AI and expert analysis to uncover anomalies and recover funds with greater accuracy and speed. By outsourcing these labor-intensive tasks, teams can focus on strategic initiatives, improve program efficiency, and achieve better financial outcomes without the operational burden.
Improve recovery outcomes
By uncovering patterns missed by traditional data mining tools
Identify overpayments, billing errors, waste & abuse
Faster, with AI analysis
Free internal teams from labor-intensive tasks
Enabling greater focus on higher-value initiatives
Customize services to your organization’s needs
From anomaly detection to fund recovery
Unlock the Full Potential of Data Mining With Advanced AI Technology
- Customizable services
Tailored to meet client-specific needs, Codoxo’s Data Mining Services provide flexible options, from detection to recovery pursuit - Expert-led analysis with AI data mining tools
Advanced AI algorithms identify anomalies, billing errors, waste, and abuse in healthcare claims with unmatched precision
- Overpayment identification & recovery
Proprietary AI detects overpayments with unmatched accuracy, outperforming traditional rules-based methods to maximize recoveries - Provider outreach & recovery pursuit
Codoxo’s team can manage recovery efforts, including communication, dispute resolution, and fund collection, using customizable templates and a secure provider portal
Identify More Recoveries & Achieve Improved Data Mining Results With Outsourced Data Mining Services
Identified
Detected
Identified
Revealed
Smarter Healthcare Cost Containment Starts With Codoxo
Data Mining Services are delivered through Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
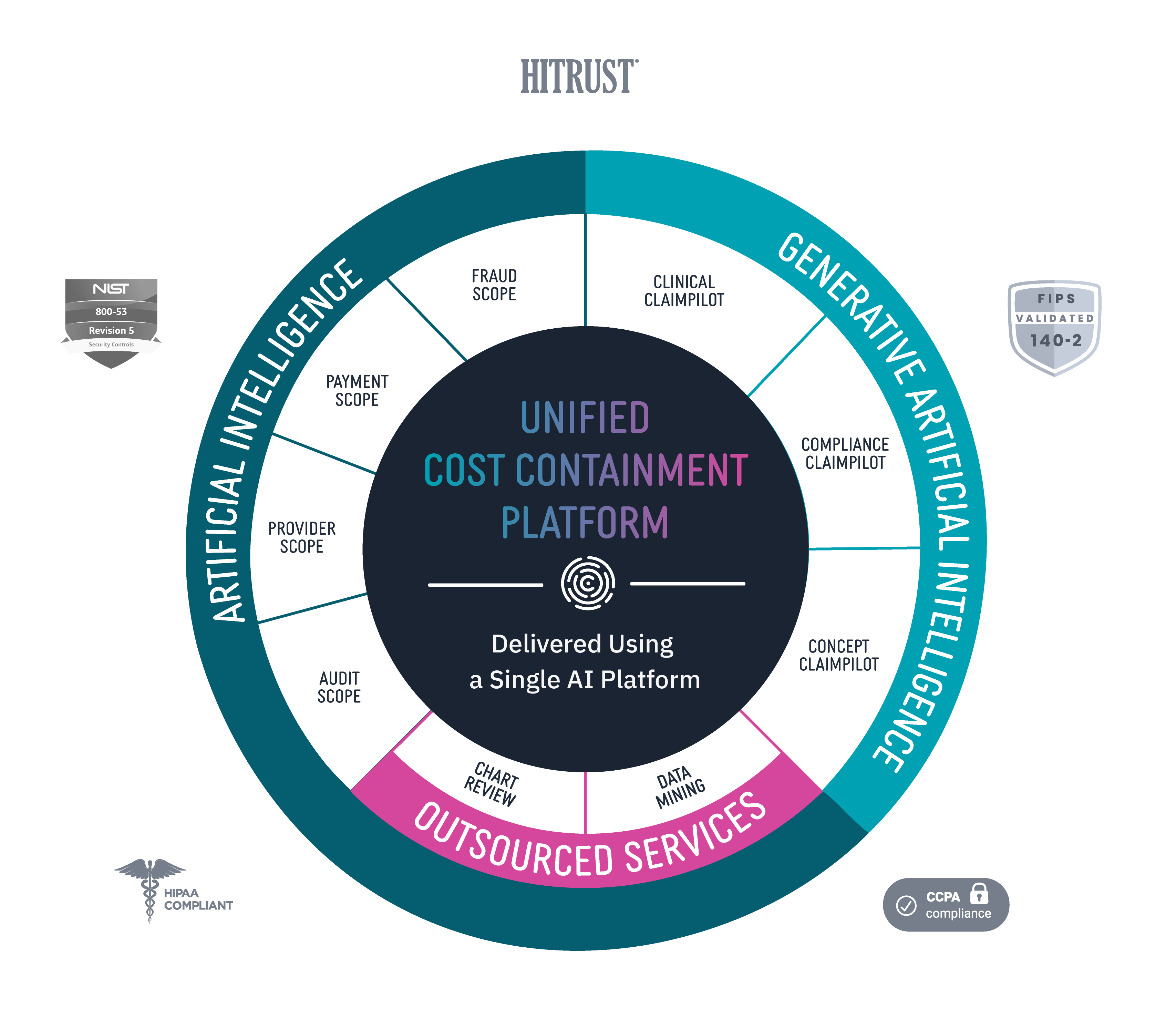
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.