Medical Record Reviews Services
Accelerate Medical Record Reviews with Generative AI for Unmatched Efficiency & Payment Accuracy

Ready to Complete Medical Record Reviews in Hours vs. Weeks?
Codoxo’s Medical Record Reviews Services help healthcare payers tackle one of healthcare’s biggest challenges: automating complex clinical reviews. By offloading this time-consuming task, including reviewing hundreds of pages of medical records and hospital bills, Codoxo relieves clinicians of administrative burdens while completing reviews faster, and with greater accuracy.
Our expert clinical auditors deliver comprehensive medical record reviews services powered by market-leading generative AI technology. From identifying potential overpayments, selecting claims for review, conducting thorough evaluations, and, when necessary, collaborating directly with providers, we can offload medical record reviews while augmenting your payment accuracy programs.
Codoxo’s medical record review services include:
- Itemized Bill Reviews
- In-patient Audits
- Facility Audits
- DRG Validation
- DRG Clinical Validation
- Short Stay
- Readmission
Unlock Faster Medical Record Reviews with Advanced AI & Gen AI-Driven Services
Operating with constrained resources, healthcare payment integrity teams are facing mounting difficulties in ensuring payment accuracy, meeting compliance standards, and handling intricate claim reviews. By outsourcing medical record reviews to Codoxo, payment integrity teams augment cost containment efforts, enhance compliance, and allow internal teams to focus on driving impactful program outcomes.
Increase recoveries
Ensure adherence to regulatory & contractual standards
With comprehensive, expert-led reviews
Manage a higher volume of reviews
Remove dollar thresholds
Free internal teams
Offload Your Payment Integrity Team While Increasing Recoveries
- End-to-end services
From detection to recovery - Comprehensive program reporting
Including audit impact analysis
- Generative AI-powered reviews
Break down barriers, streamlining the challenges of traditional manual review processes
Break the Status Quo with Codoxo’s Medical Record Reviews Services
immediate impact on both prepay and postpay programs
Smarter Healthcare Cost Containment Starts With Codoxo
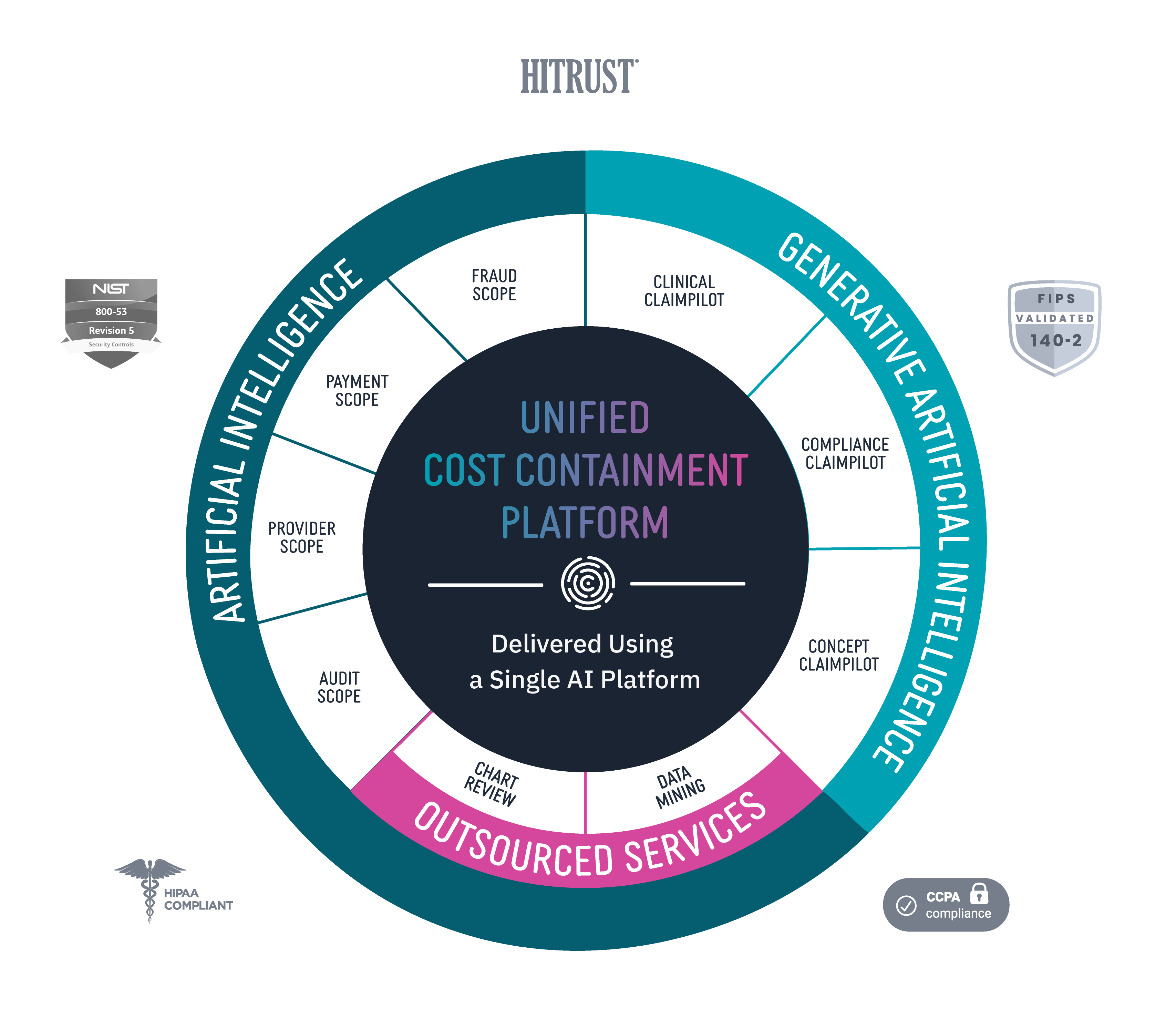
Medical Record Reviews Services are delivered through Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and operational optimization. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more efficient.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services