Maximize Recoveries With the Power of Generative AI Across Healthcare Audits & Data Mining
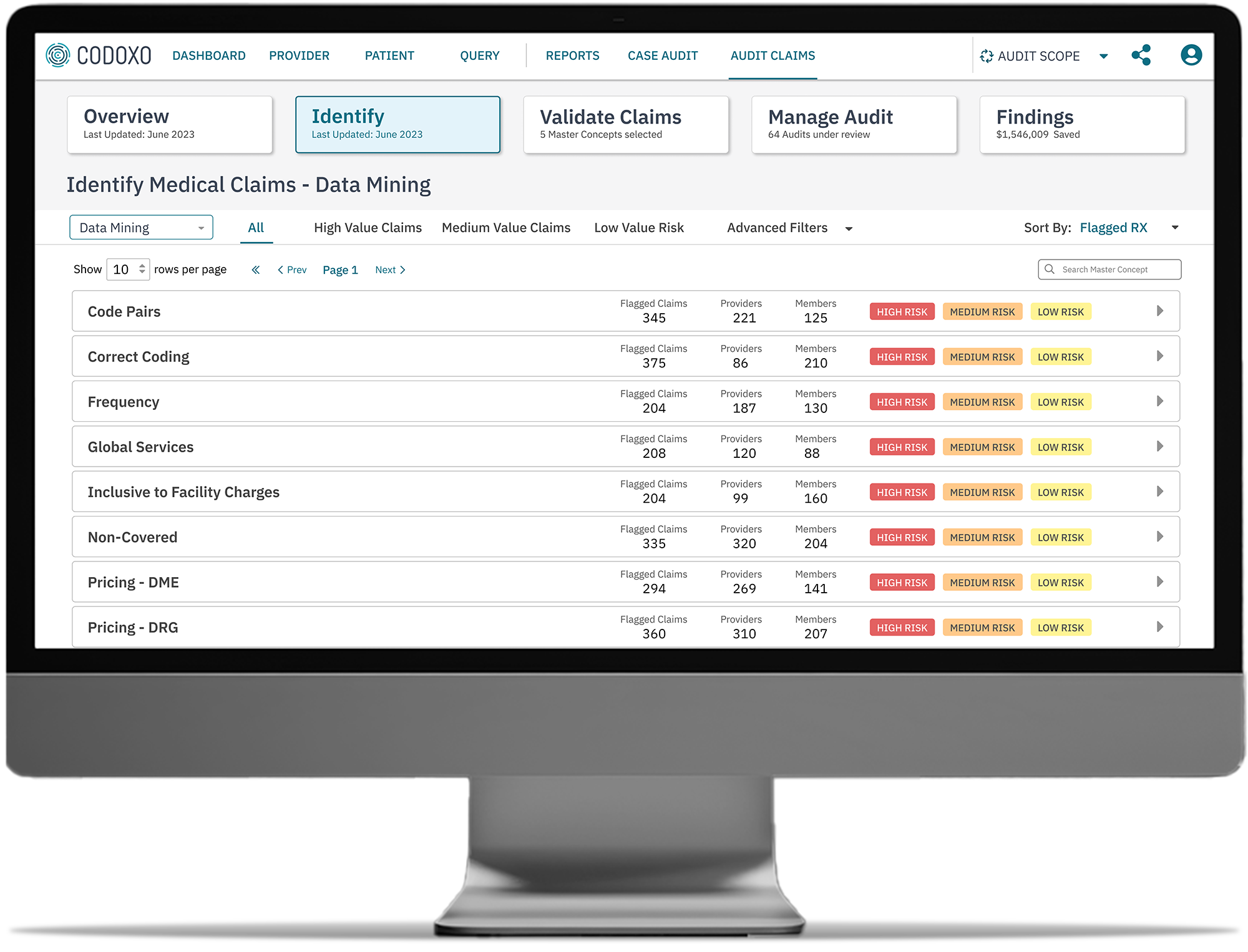
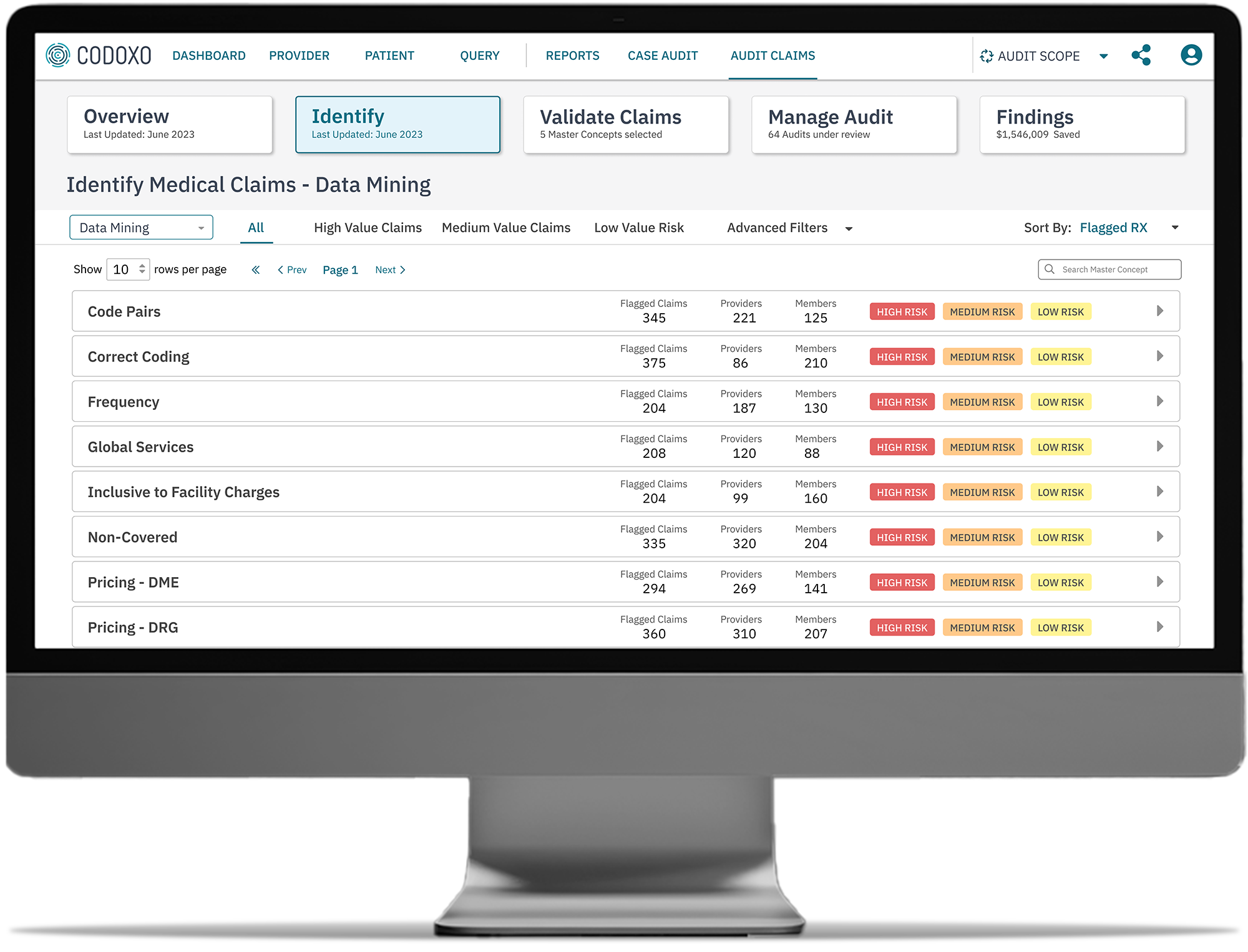
Say goodbye to manual, labor-intensive medical claims audits. Audit Scope drives powerful automation and efficiency, transforming medical and pharmacy claims audits and data mining for improved payment accuracy.
Ready to Save $32 Per Member Per Year?
Audit Scope
Audit Scope is a cutting-edge audit workflow and automation platform that leverages generative AI to transform healthcare audits, audit case management, and healthcare data mining. By automating high-risk claim identification and streamlining medical record and pharmacy reviews, Audit Scope augments human auditors and drives exponential efficiencies.
This allows healthcare payers to focus on high-impact activities that maximize financial recovery and ensure healthcare payment accuracy from pre-claim submissions to postpay.

Improve Healthcare Payment Accuracy With Generative AI for Healthcare Audits
By infusing generative AI into audit, case management, and data mining workflows, Audit Scope equips payment integrity teams to minimize the risk of overpayments and potential financial exposure.
Quickly & accurately flag claims
For audit and data mining selections for further review
Expedite healthcare audit reviews
With generative AI-assisted workflows for faster determination across medical and pharmacy claims
Analyze broad claim sets with unparalleled accuracy
For the most comprehensive view of outlier claims and improper payments
Share powerful reporting & insights
With payment integrity teams, FWA investigators, and government agencies to fuel greater healthcare compliance
Enhanced payment validation
By comparing medical records against policies to verify correct payments and safeguard against errors
A Game Changer for Audit & Data Mining Teams
Audit Scope expedites the audit process with its generative AI-powered workflows, streamlining case management, and empowering audit teams to manage every aspect of an audit seamlessly in one platform.
- Identify audits using AI
Leverage AI and novel PI rules for the most accurate claim selection across medical and pharmacy claims - Seamless review summaries
Effortlessly access review summaries and the rationale for claim selections directly within existing workflows - Streamlined medical record reviews
Utilize built-in capabilities, including a provider portal, to enable electronic submission of medical records directly into audit cases - Direct access to source documents
Confirm and review required information with ease by referencing essential documents in real-time - Comprehensive workflow integration
Streamline every stage of the audit process with a comprehensive, unified system. From audit selection and lifecycle management to provider communications, effortlessly handle financials, recoveries, findings, and reporting—all in one place
- Dynamic policy adaptability
Quickly identify emerging schemes or changes in policies, ensuring healthcare audits remain accurate and relevant - Intuitive interface with deeper insights
Gain actionable insights into fraud schemes through an easy-to-navigate interface, powerful query tools, and clear explanations of fraud patterns - Customizable reporting
Design tailored reports to meet strict healthcare compliance and regulatory requirements with precision and clarity - Automated communication tools
Leverage built-in templates for audit notifications, findings, and appeal responses to streamline provider communications and ensure healthcare compliance
Uplevel Your Healthcare Compliance with Audit Scope
$32 PMPY
average savings
$25 million
Over $6 million
in total paid exposure identified for a single pharmacy, supporting healthcare compliance initiatives
Faster
Smarter Healthcare Cost Containment Starts With Codoxo
Audit Scope is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI and generative AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform Products & Services
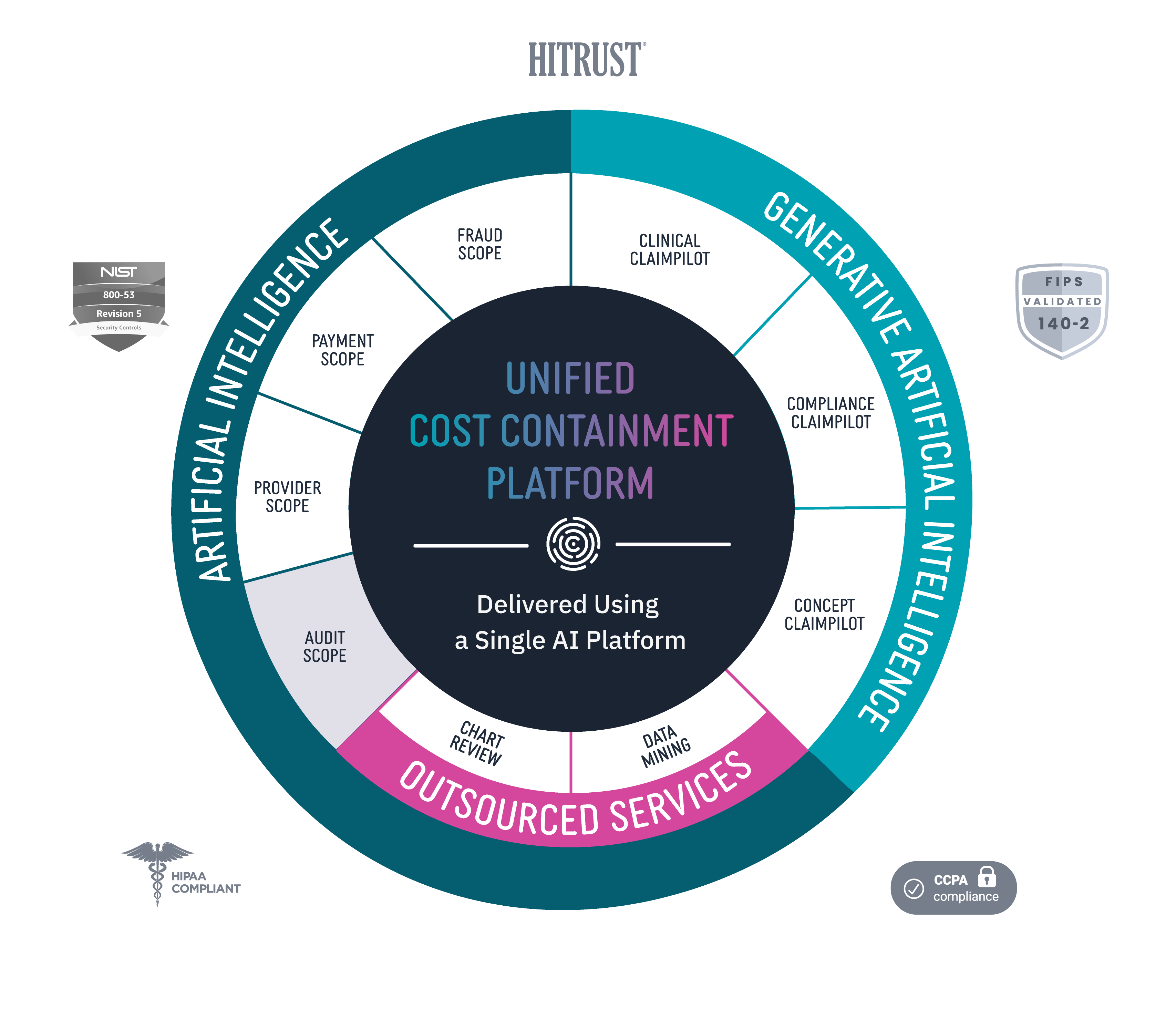
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.