Generative AI That Transforms Your Payment Integrity Outcomes
Boost Efficiency for PI and SIU teams by 20x to 30x with ClaimPilot.
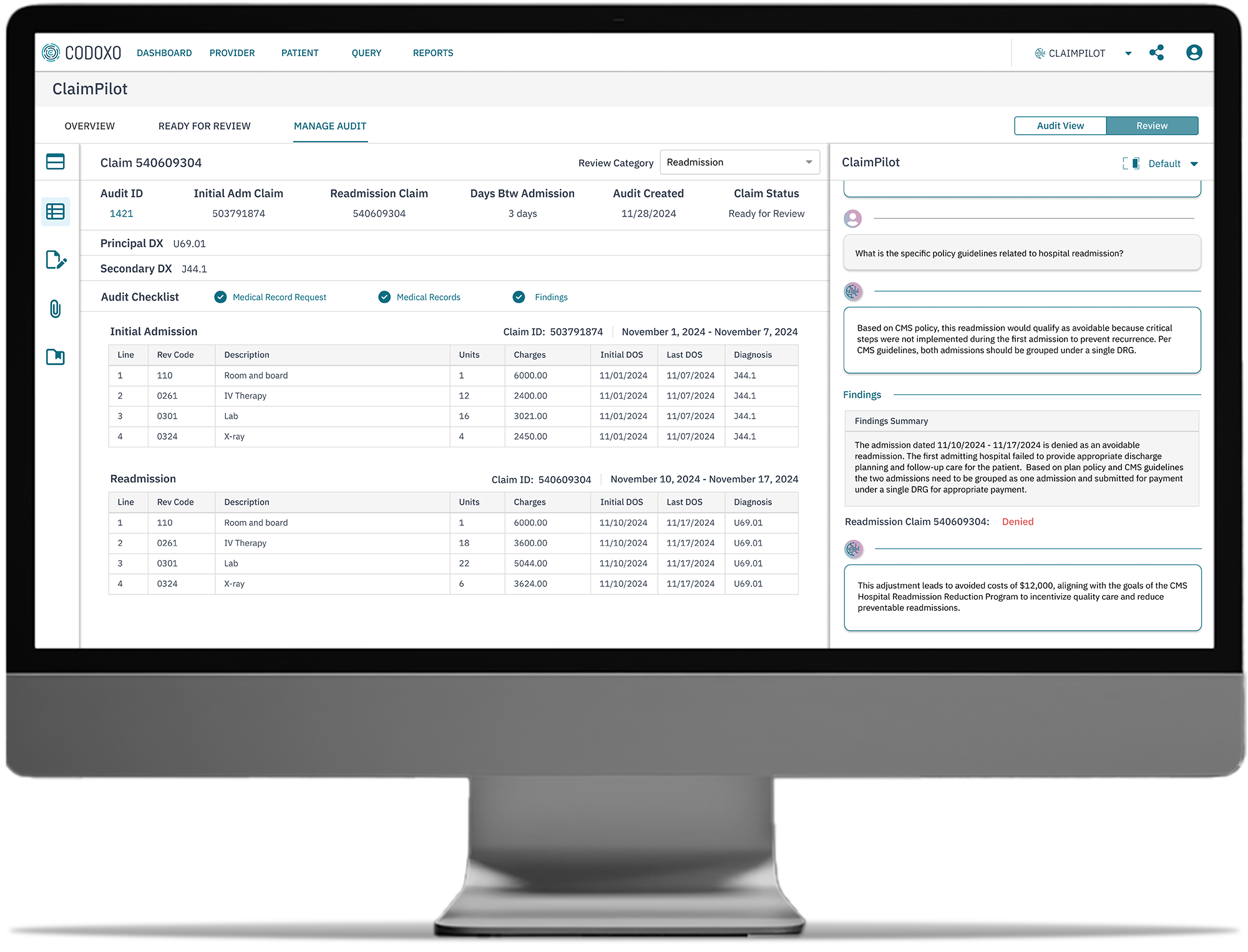
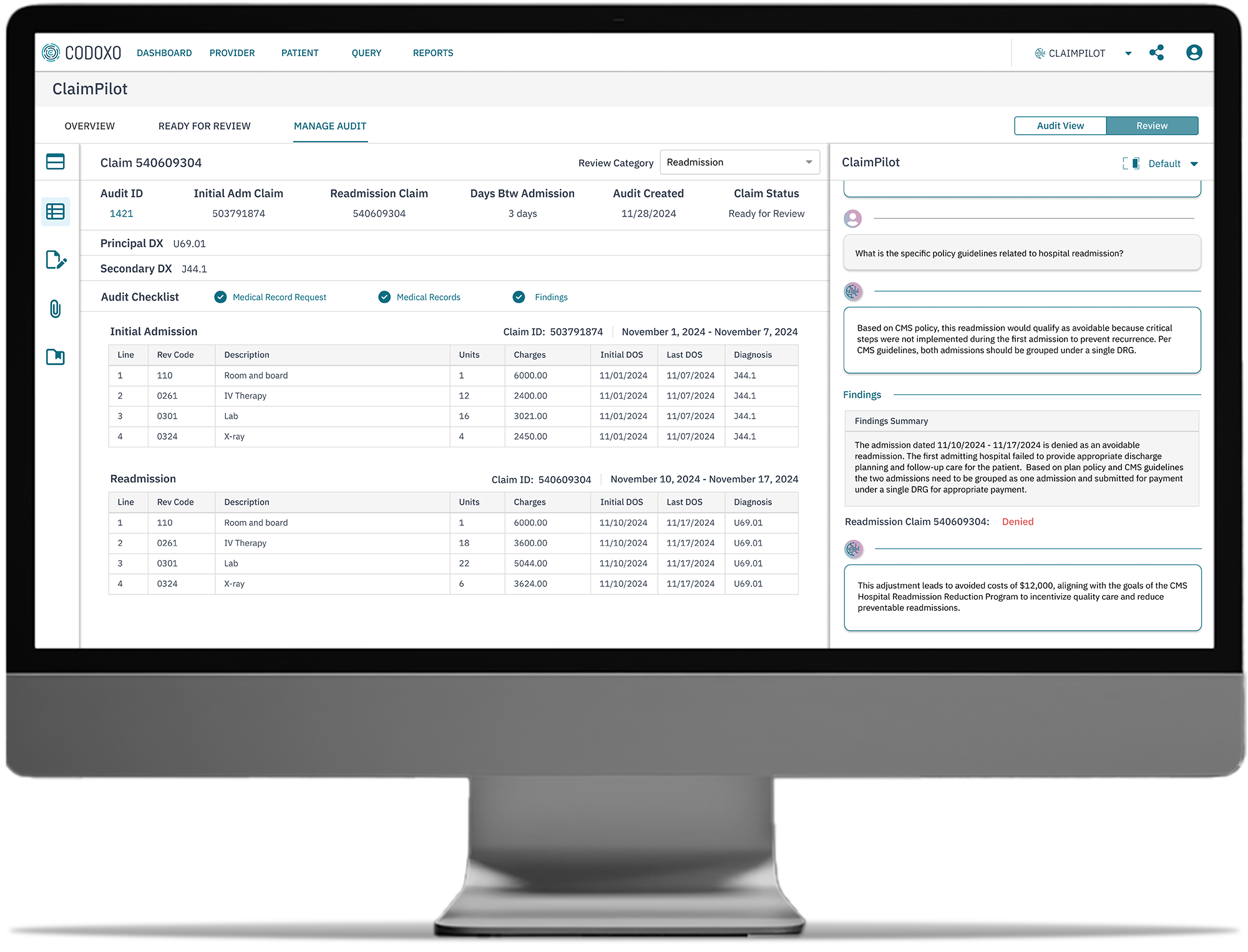
ClaimPilot
As the latest advancement in Codoxo’s award-winning Unified Cost Containment Platform, ClaimPilot seamlessly integrates across payment integrity and healthcare fraud, waste, and abuse solutions, offering unparalleled automation, resource efficiencies, and best-in-class security.
ClaimPilot Suite of Generative AI Solutions

Automate. Elevate. Protect.
ClaimPilot empowers healthcare payers, agencies, and pharmacy benefits managers to reimagine payment integrity.
Generative AI-powered automation
Streamline complex and repetitive tasks, letting your team focus on what matters most
Exponential resource efficiencies
Elevate productivity across Payment Integrity, SIU, Claim Operations, Legal/Compliance, Provider Services, and Clinical teams
Best-in-class security
Safeguard sensitive data with robust, industry-leading protections
Enhanced accuracy & reliability
Reduce human error and achieve precise claims data analysis
Smarter Healthcare Cost Containment Starts With Codoxo
ClaimPilot is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI and generative AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
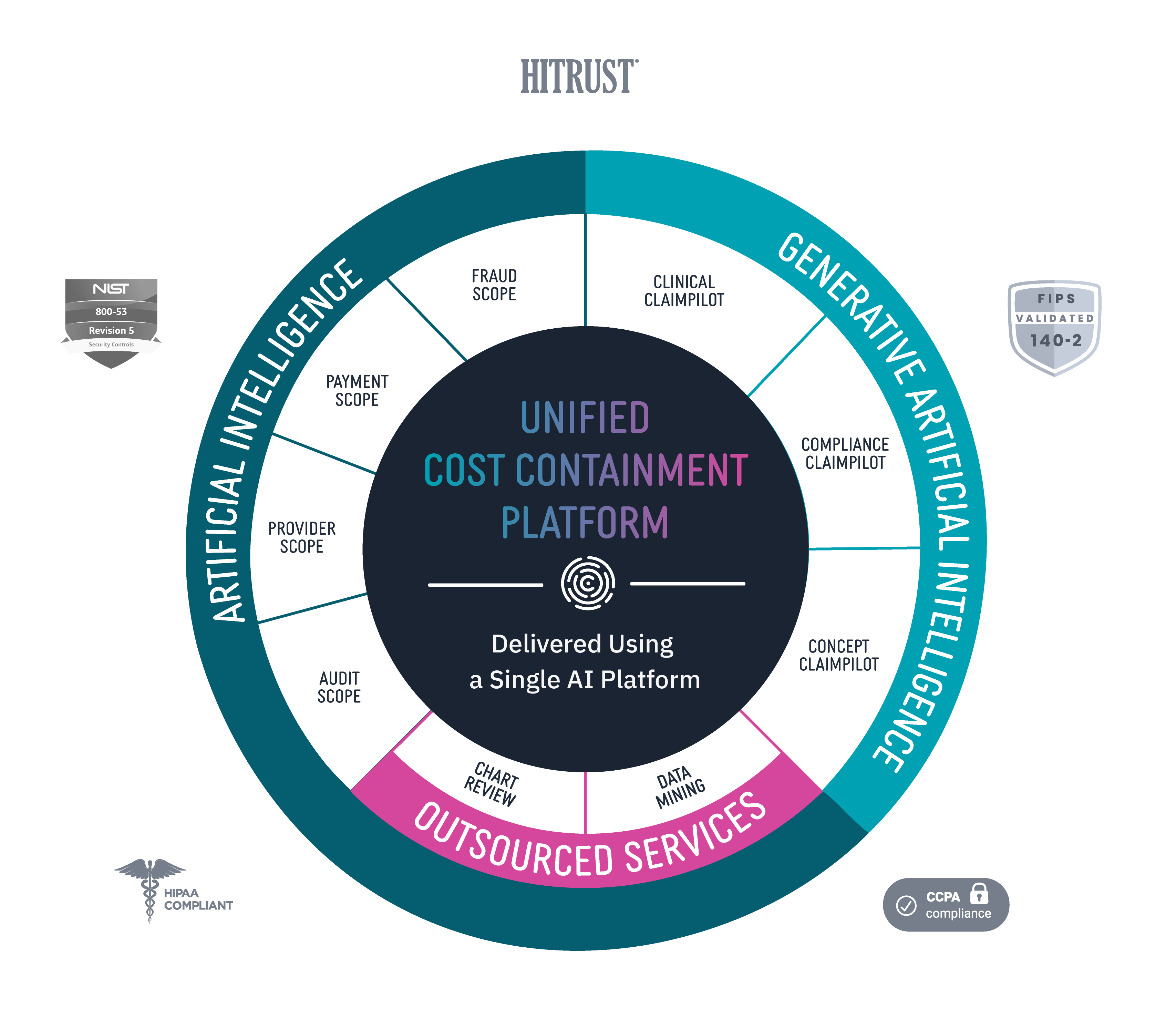
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.