Supercharge Medical Record Reviews with Gen AI for Unmatched Audit Efficiency & Accuracy
Ready to Complete Medical Record Reviews in 24 Hours or Less?
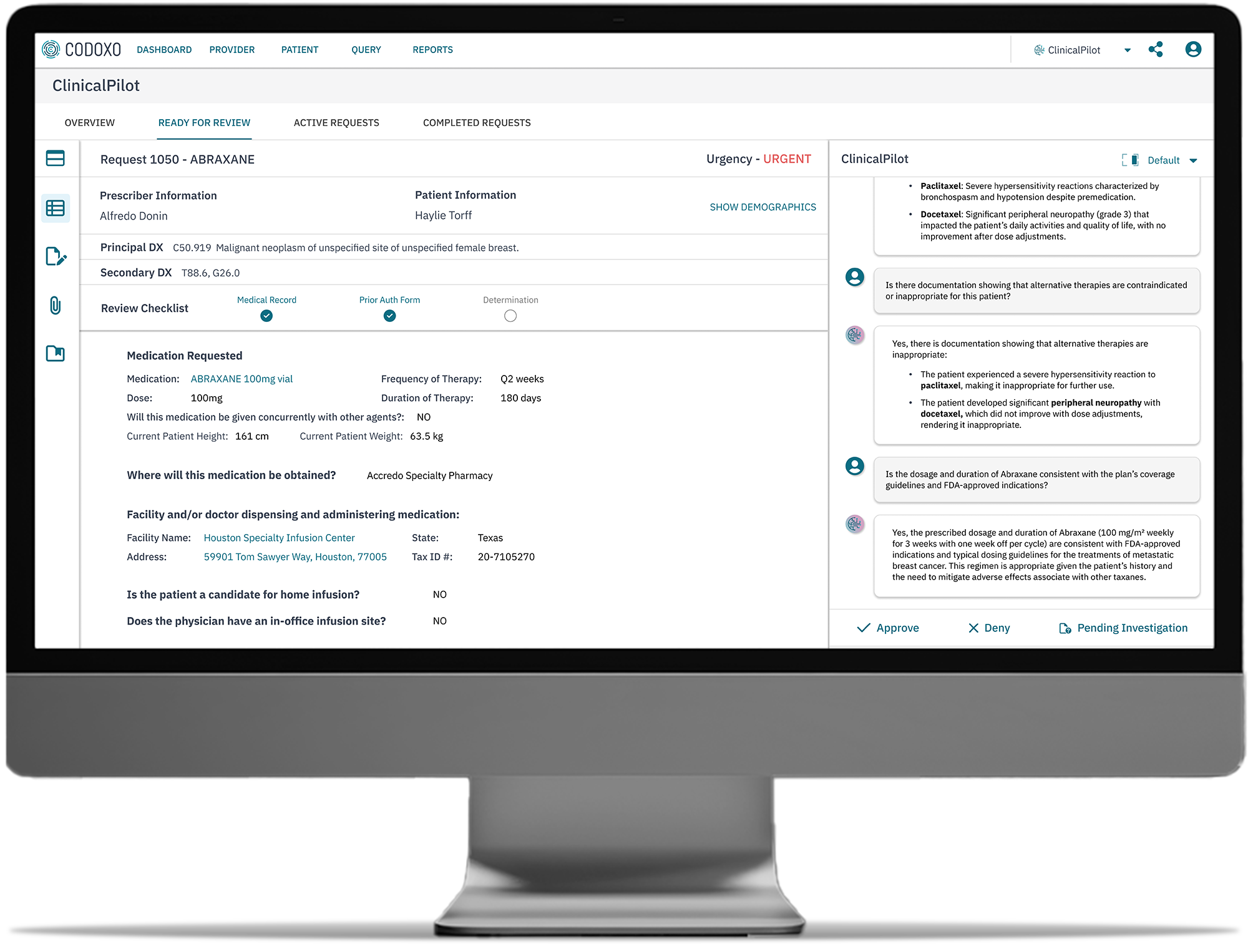
Clinical ClaimPilot
Clinical ClaimPilot addresses one of healthcare’s most complex challenges – automating complex medical record reviews, including DRG reviews, which account for up to 45% of healthcare costs.
Clinicians are tasked with the arduous job of reviewing granular and lengthy medical records and hospital bills for complex clinical reviews, often hundreds of pages long, diverting their focus away from patient care. This takes a toll on workforce morale and wellness.
Next-level automation frees clinicians and administrators to focus more strategically. In turn, health organizations can do more with the resources they already have.
Generative AI-driven audits deliver exponential efficiency gains across:
-
- Itemized bill reviews
- In-patient audits
- Facility audits
- DRG validation
- DRG clinical validation
- Short stay
- Readmission

Faster Turnaround Times for Clinical Audits, Powered By Generative AI
Most healthcare payers perform in-patient and facility claim audits selectively (limited to high dollar thresholds); manually (requiring clinician review); and slowly (often taking 1-3 weeks to review a single audit) – until now.
Faster audit turnaround times
Exponentially speed medical record reviews from weeks to hours
Eliminate dollar thresholds
Review, audit, or investigate any and all claims regardless of dollar value
Rapid deployment
No need for specialized technical support
Power Complex Claim Audits With Generative AI for Faster, More Efficient Reviews
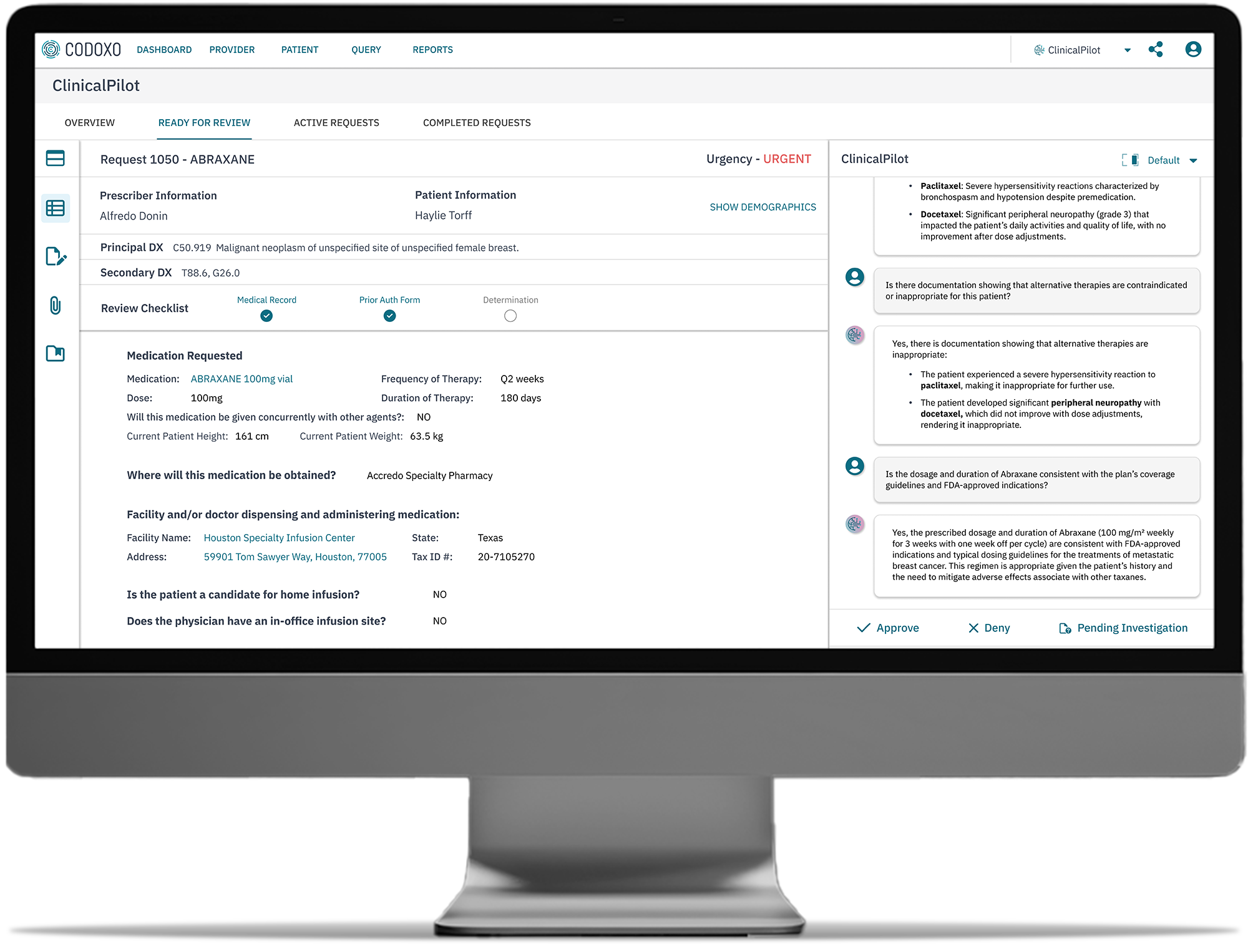
Clinical ClaimPilot expedites the audit review process by automating medical record reviews and providing auditors everything they need to complete the audit at their fingertips. The platform identifies claims for audit and organizes them within clear audit categories, such as DRG reviews, readmissions, or itemized bill reviews. Within each audit, the auditor receives a review summary provided by Clinical ClaimPilot including the reason(s) for audit selection and all required documentation including medical records, itemized bills, etc. needed to make a determination.
- Integrated medical record requests
See if a medical record request has been sent and whether the provider has uploaded the necessary documentation, including ability to send a record request - Organized review categories
Claims are categorized for easy navigation and streamlined auditing processes - Detailed claim information
View essential claim details, including DRG codes, diagnosis, paid amounts, and allowed amounts - On-demand, intuitive dashboard
Displays a summary of activities since the last login, including newly identified claims and those not reviewed due to contractual limits
- Findings note feature
Log findings and recommendations during the audit process, including suggested diagnosis changes and their implications on reimbursement rates - Access to source documentation
Quickly navigate to the original source documents for all claim information, enhancing transparency and traceability - Audit impact analysis
Calculate and display potential overpayments or adjustments resulting from claim findings
Immediate Impact to Prepay and Postpay Programs
Reduces
audit and medical record review turnaround times from days to less than 24 hours
Increases
Scales
audit programs and enhances payment accuracy across all claim types
Improves
Streamlines
Delivers
Smarter Healthcare Cost Containment Starts With Codoxo
Clinical ClaimPilot is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Clinical ClaimPilot is part of Codoxo’s ClaimPilot suite of Generative AI-driven payment integrity solutions, including:
Explore Codoxo’s Unified Cost Containment Platform Products & Services
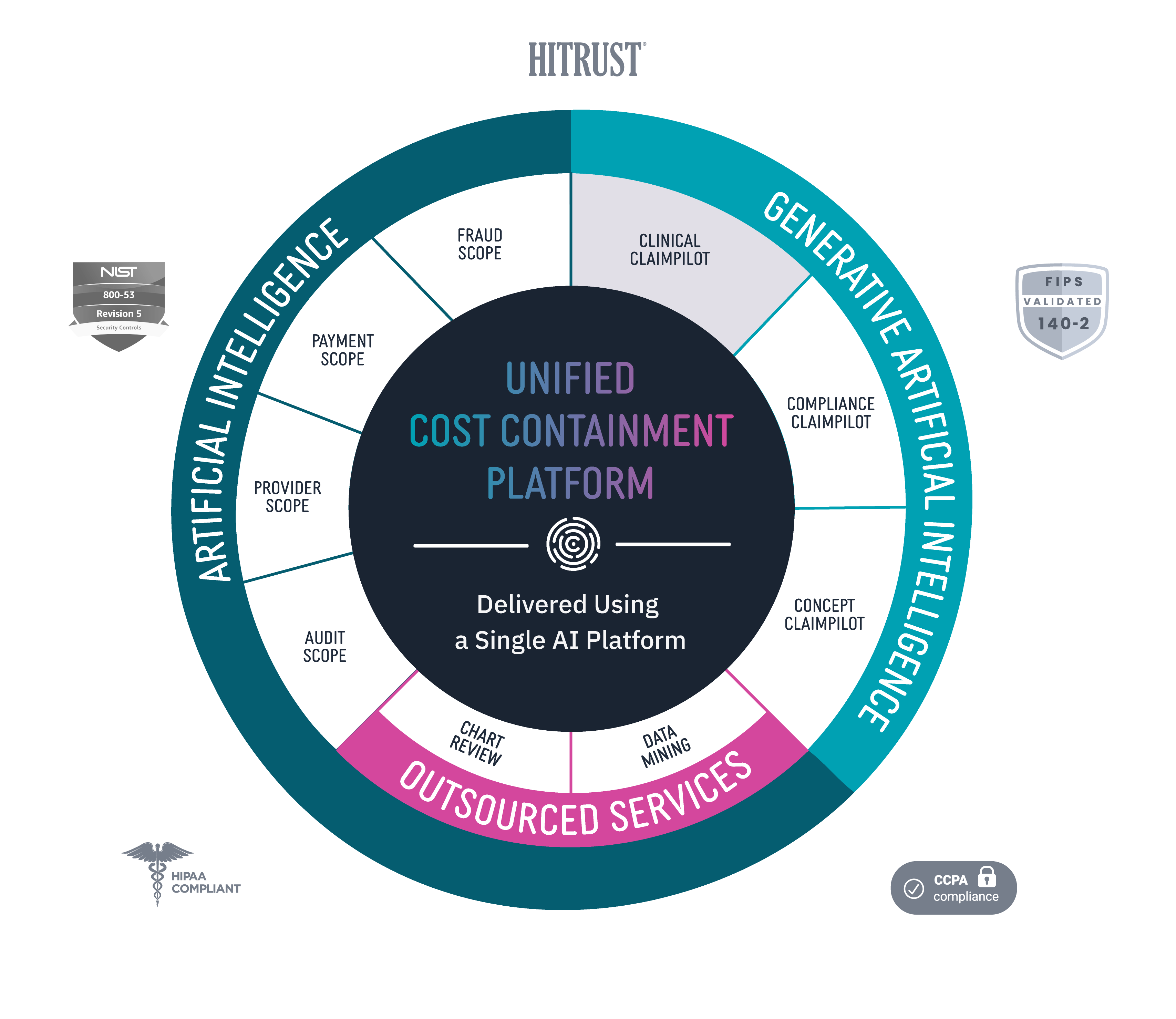
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.