Generative AI-Powered Solutions for Early Payment Integrity Intervention
Pioneer the future of healthcare cost containment with Codoxo’s generative AI solutions – where provider abrasion is minimized, savings are optimized, and recoveries are maximized.
Codoxo’s cost containment solutions strengthen payment integrity programs by identifying and addressing issues early in the process.
Ready to Save $60 PMPY?
Discover the Power of Early Intervention.
Move Your Payment Integrity & Cost Containment Programs Upstream
Explore Codoxo’s Cost Containment Solutions
Manage Improved Payment Integrity Outcomes With Ease & Confidence
Embrace a seismic shift left
Stop financial loss pre-claim with more accurate healthcare payments
Analyze all claim types
Professional, facility, pharmacy, behavioral, dental, and workers comp – to create connections across data and identify patterns at every level, from individual claims and providers up through groups, networks, and plans
Empower stakeholders & teams
Operate at the top of their licenses and focus on higher-value tasks
Boost automation, streamline workflows, & enhance process efficiency
Gen AI technology reduces manual labor and identifies schemes with greater speed and accuracy
Strengthen healthcare compliance
AI-powered auditing ensures accurate documentation, maintains regulatory standards, and provides clear audit trails for all audits
Trust best-in-class security
Codoxo’s security standards will protect your data at the highest levels industry-wide
Not All AI-Driven Solutions for Payment Integrity Are Created Equal
$60 PMPY
20x-30x
90% gains
in payment errors, improving accuracy and reducing manual intervention
Up to 40%
Smarter Healthcare Cost Containment
Starts With Codoxo
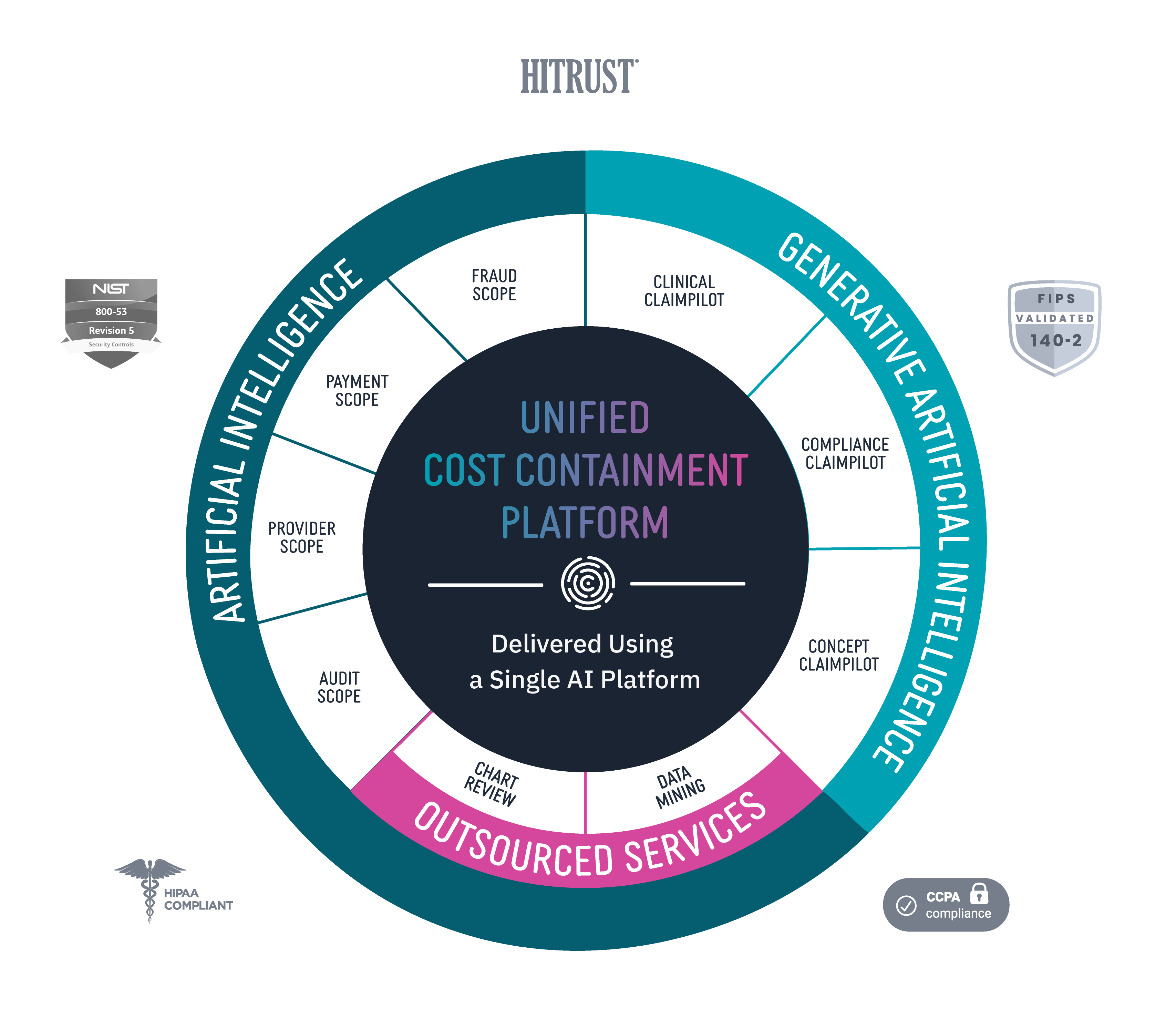
Codoxo’s products, services, and solutions are delivered through our Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced healthcare fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services