Proactive Shift Left Strategy
The Key to Minimizing Provider Abrasion & Maximizing Savings with AI-Driven Provider Education
The only platform and provider portal designed to proactively engage providers at the earliest stages of the payment process, using advanced AI to deliver targeted education that reduces claim denials, prevents payment delays, and strengthens provider relationships.
Unlock $8-12 PMPY in Proven Savings through Provider Education. See How.
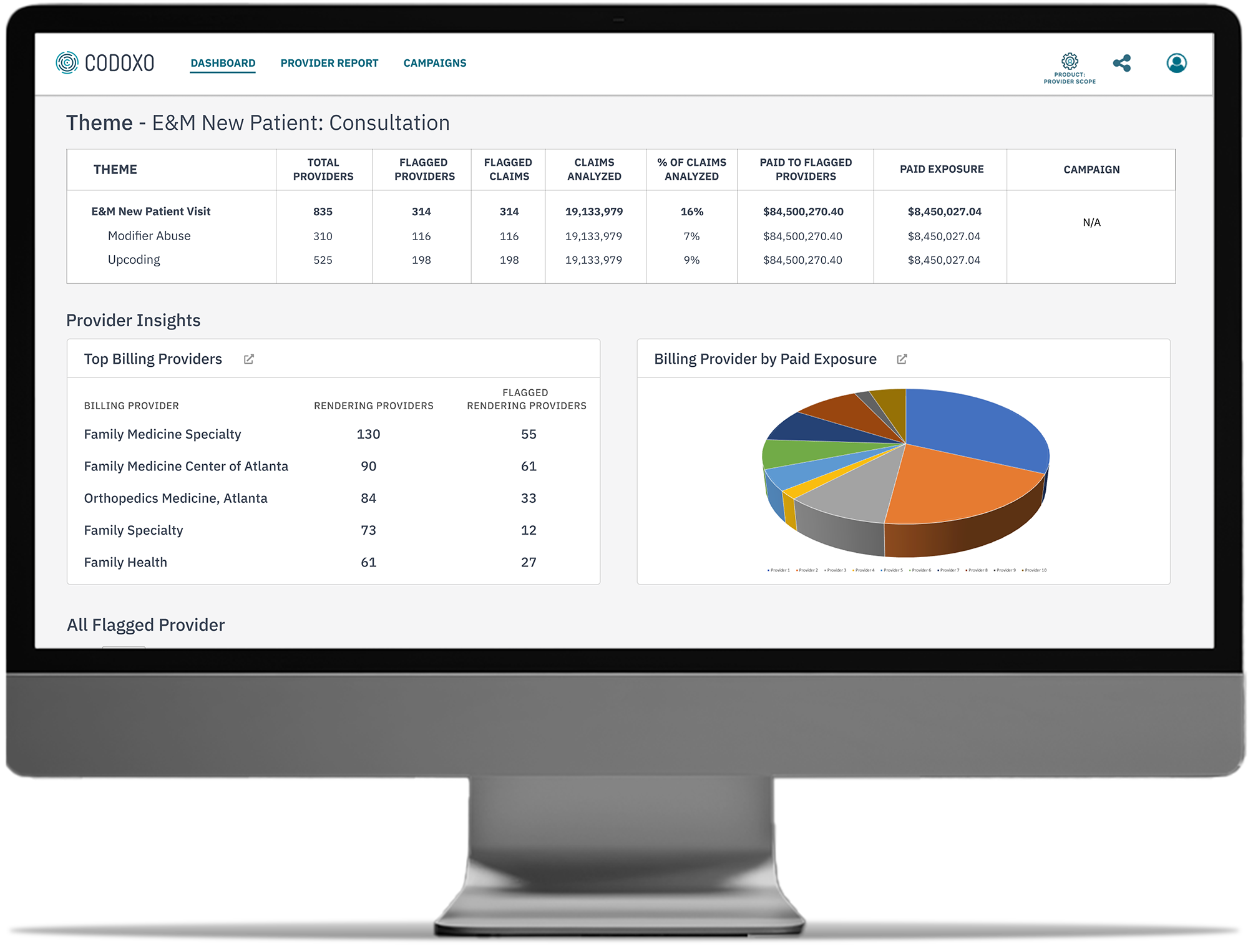
Provider Scope & Provider Portal
By addressing billing and coding issues before claims are submitted, Provider Scope and its provider portal ensures accurate coding and payments while minimizing friction between payers and providers.
The platform leverages a dedicated provider portal to share coding and billing performance, enabling providers to self-monitor and adjust their billing practices. This proactive approach eliminates the need for manual interventions or burdensome audits, empowering your network to achieve provider compliance and avoid errors effortlessly.

Enhance Billing Accuracy & Reduce Friction With AI-Driven Provider Education & Portal
Provider Scope’s unique combination of early intervention, transparent reporting – plus dedicated provider portal – optimizes provider billing performance, engagement, and cost avoidance.
Real-time peer benchmarking reports
That enable providers to self-correct
Lower pre-claim submission costs
Through automated education and early intervention for the greatest cost avoidance and savings
Proactive monitoring with self-service tools
Leads to reduced provider abrasion
Payer-provider shared access
To performance data through a holistic platform
Rapid provider performance insights
Across the entire network
Build trust with providers
Improve billing practices through ongoing training and reporting
Streamline Provider Billing with Cutting-Edge AI Tools
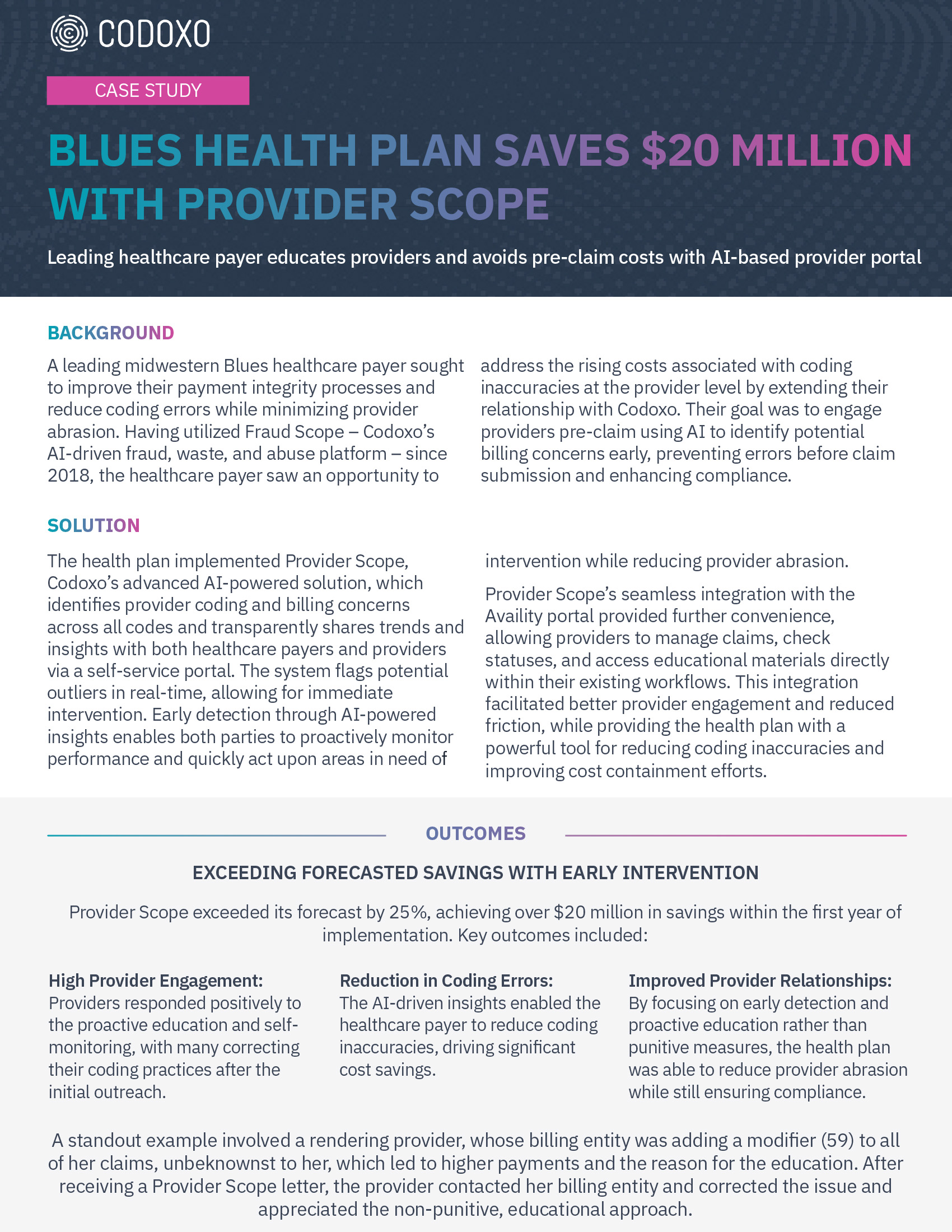
With its AI-driven workflows and focus on pre-claim submission education and insights, Provider Scope not only reduces prepay costs but strengthens payer-provider relationships through more accurate claim submissions and payment integrity.
- Provider portal for self-monitoring, peer comparison & communication
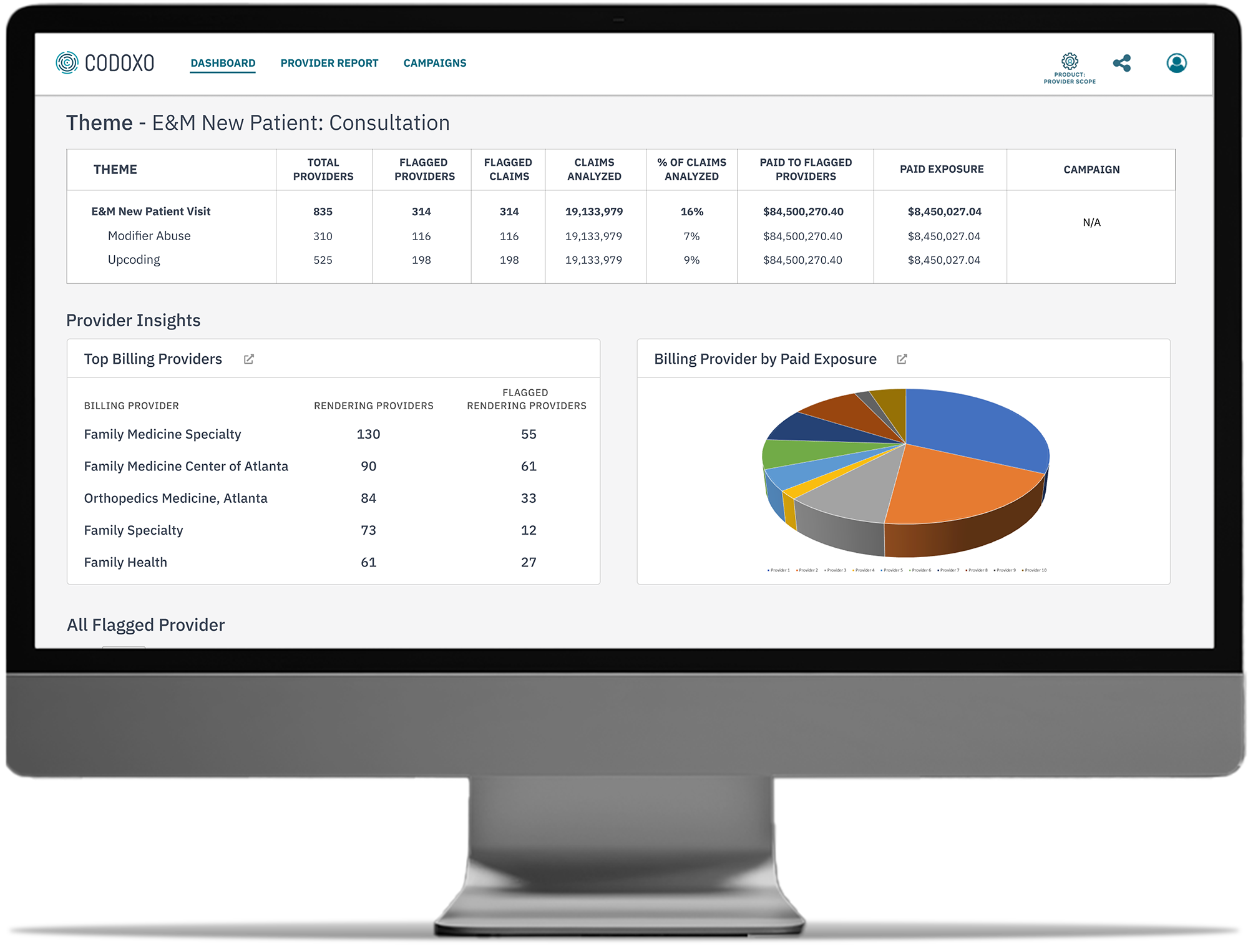
Our portal lets providers compare coding practices with peers, improving transparency, engagement, and reducing provider abrasion. - Identifies provider billing & coding concerns
AI analyzes post-payment claims, coding, and prepayment processes to identify themes and providers in need of education through easy-to-interpret comparative charts. - Automates proactive provider education programs
Flagged providers receive automated, customized outreach related to outlier behavior with guidance to improve claim integrity.
- Exponentially more themes for identifying outlier behavior
Provider Scope offers exponentially more themes than traditional methods, resulting in more cost avoidance opportunities. - Ongoing program monitoring & detailed reporting
Alerts, follow-ups, and reports keep providers informed and compliant, while performance charts give payers clear insights into program outcomes. - Dedicated support from certified coding staff
Providers gain access to expert guidance on billing patterns and best practices, ensuring greater compliance.
Faster Time to Implementation, Faster Time to Savings
$6-12 PMPY
in cost avoidance
Up to 40%
90%
Smarter Healthcare Cost Containment Starts With Codoxo
Provider Scope is part of Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
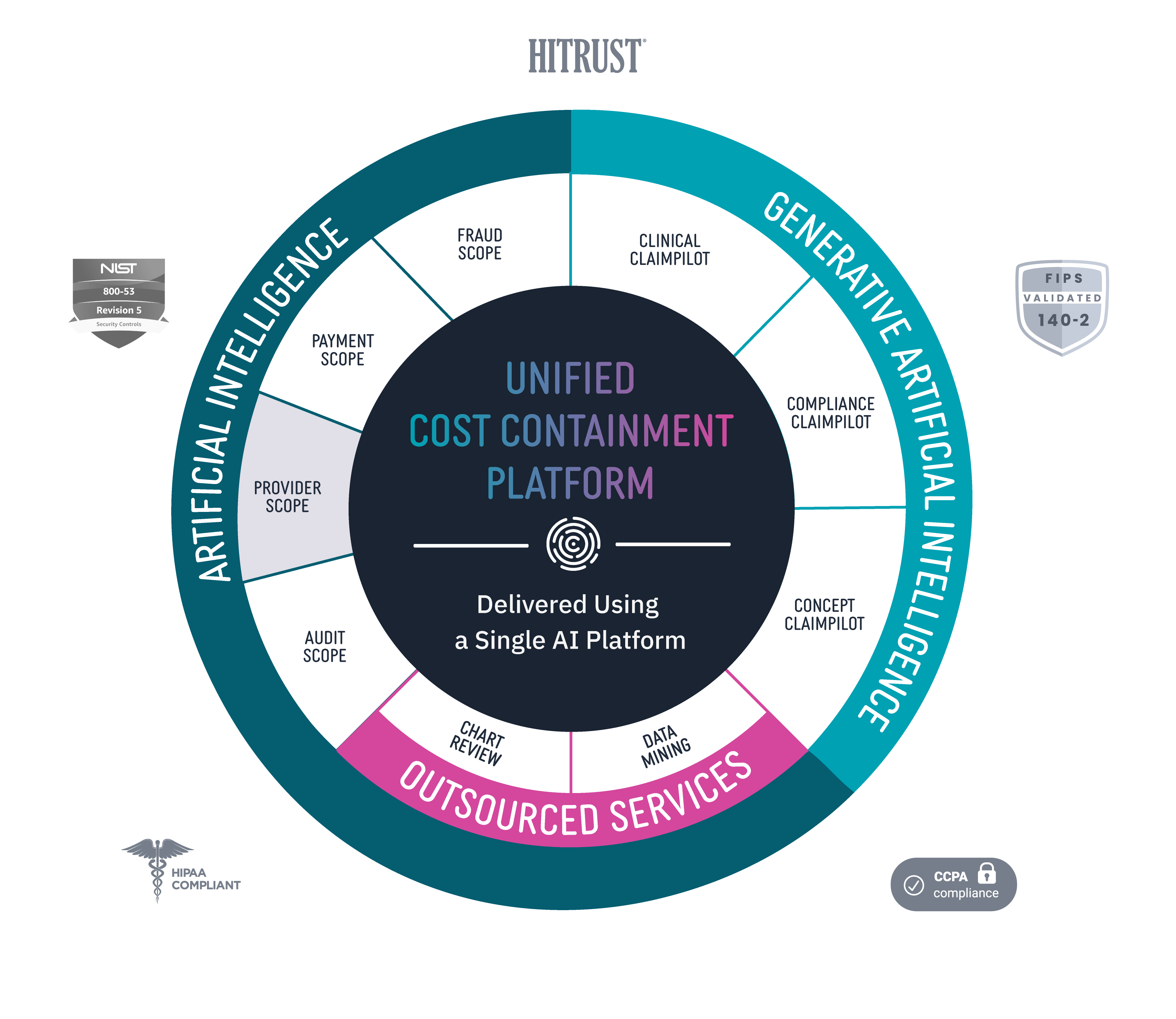
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.