The Earliest Payment Integrity Intervention on the Market
Codoxo’s platform shifts payment integrity programs further upstream than even prepay while minimizing disruptions for your providers.
Discover How Our Partner Achieved 99% Payment Accuracy, Minimized Errors, & Eliminated the Need for Manual Intervention
Proudly reducing healthcare costs for
and trusted by top healthcare payers, government agencies, and pharmacy benefit managers (PBM/PBAs)
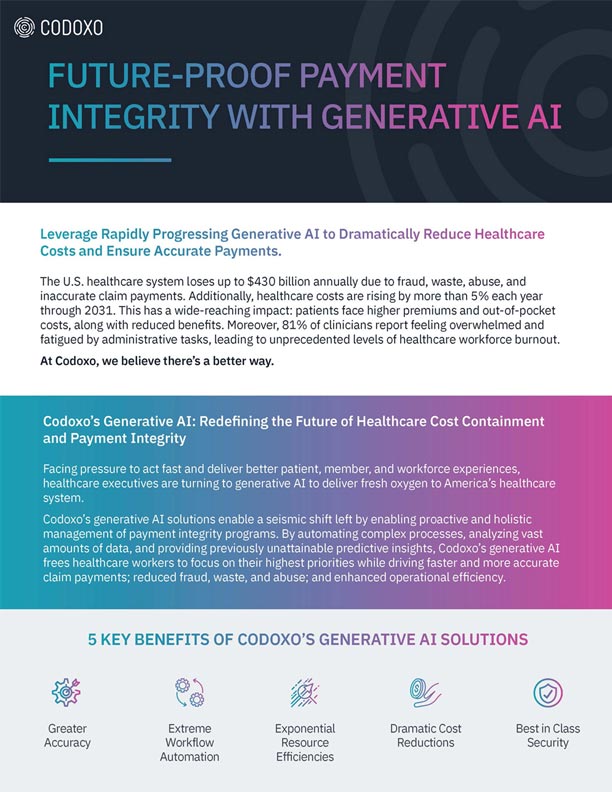
Unified Cost Containment Platform
Codoxo’s Unified Cost Containment Platform leverages generative AI and advanced automation to shift left in the payment cycle, enabling earlier intervention, proactive cost avoidance, and stronger provider relationships—all within a single, unified platform.

Eliminate Silos. Maximize Collaboration. Amplify Results.
Working in disconnected teams is a thing of the past. Codoxo’s platform unites departments and empowers your entire organization with a single source of truth for healthcare cost containment.
Shift payment integrity programs upstream
To proactively prevent financial losses before they occur by impacting claims before they are created by providers
Dramatic cost savings & avoidance
With faster and more comprehensive claim analysis
Exponential workforce efficiency
By eliminating repetitive tasks with generative AI that identifies problem areas faster and more accurately
Reduce provider abrasion
By reducing denials, payment delays, and lengthy audits
Maximum recoveries
Through proactive fraud, waste, and abuse prevention
Best-in-class security
Safeguarding your organization at every step
Codoxo Delivers Results
payment accuracy, reducing errors and manual intervention
workforce efficiency for payment integrity and SIU teams
The Industry’s Most Advanced Features
- Unified data views
One platform for cross-team collaboration and transparency - Generative + self-learning AI
A proprietary mix of technologies tailored for healthcare - Automation at scale
Reduce labor-intensive tasks across audits, case management, and compliance
- Intelligent reporting
Customizable, prescriptive insights to stay ahead of emerging trends - Real-time access
Improve decision-making with instant data availability - Rapid onboarding
Start realizing savings in weeks, not months
Move Payment Integrity Programs Upstream – A Smarter Way to Manage Healthcare Costs & Provider Relationships
Codoxo’s Unified Cost Containment Platform is a single platform enabling teams to work cohesively across pre-claim, prepayment and postpayment activity, including provider education, payment integrity, SIU, and network management.
The platform analyzes all types of claims and codes for the most proactive identification of existing or emerging areas of concern. Empower your team to engage as early as possible to avoid disruptions to provider workflows and ensure accurate payments the first time.
Smarter Healthcare Cost Containment
Starts With Codoxo
Codoxo’s products, services, and solutions are delivered through the Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift further left than prepay by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform Products & Services
Codoxo’s Unified Cost Containment Platform leverages generative AI and advanced automation to shift left in the payment cycle, enabling earlier intervention, proactive cost avoidance, and stronger provider relationships—all within a single, unified platform.
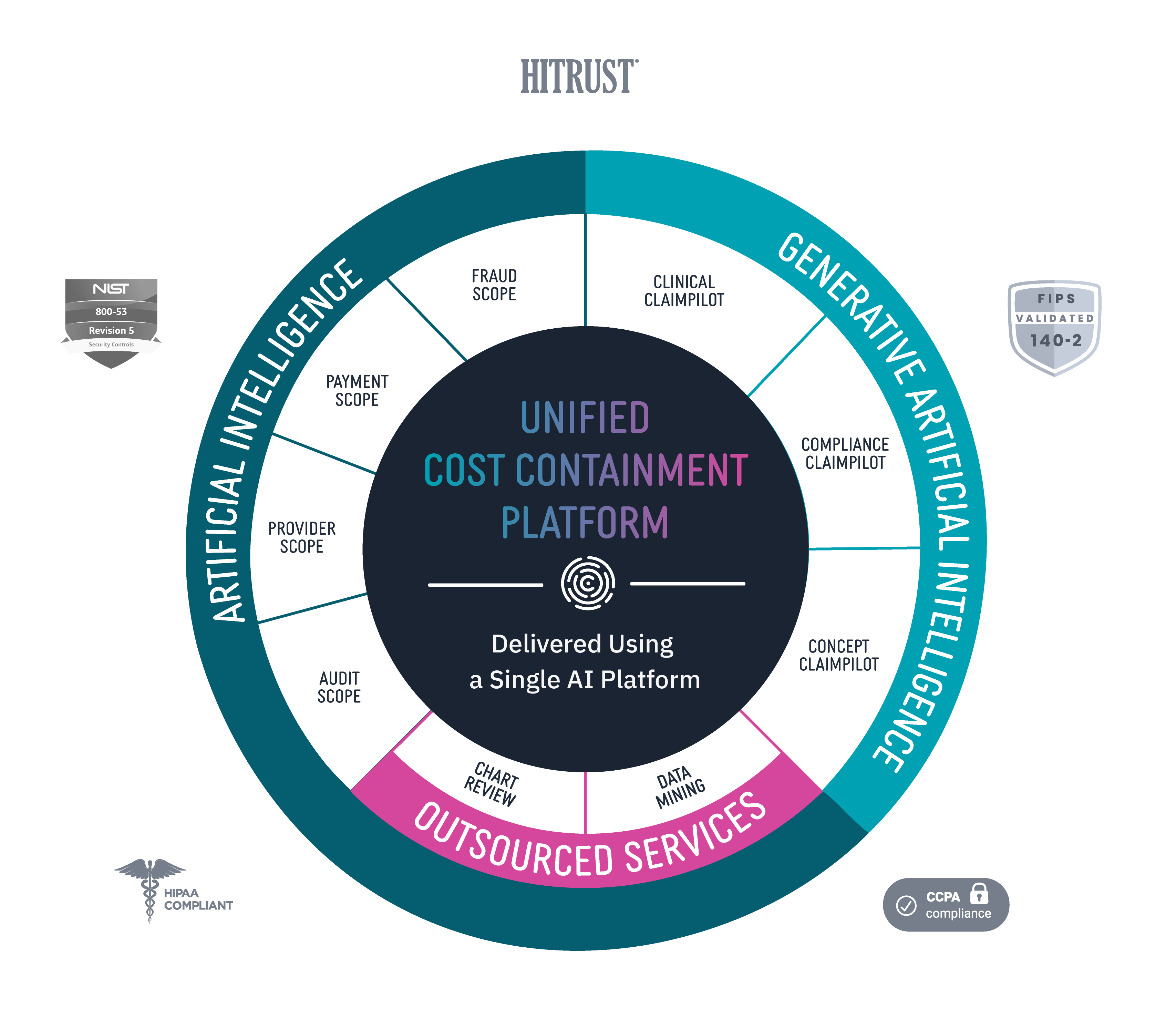
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.