Virtual SIU Services
Increase Recoveries While Scaling SIU Operations through AI-Driven Outsourced SIU Services

Ready to Realize 3X ROI with Codoxo’s Fraud Investigation Services?
Codoxo’s Virtual SIU Services enable healthcare payers, PBMs and state agencies to scale their operations while ensuring compliance with fraud, waste, and abuse (FWA) regulations. By outsourcing key SIU functions, organizations can enhance their ability to detect and investigate suspicious activities faster and more effectively.
Our onshore team of experts, including Certified Fraud Examiners (CFE), Accredited Health Care Fraud Investigators (AHFI), Certified Professional Coders (CPC), Registered Nurses (RN), Certified Pharmacy Technicians (CPhT), and Certified Dental Coders (CDC), work seamlessly with your internal team using Codoxo’s AI-driven Unified Cost Containment Platform to identify leads, create and manage cases, and provide timely reporting.
Scale Operations While Ensuring Compliance With Virtual SIU Services
Maximize savings
With quick, proactive AI detection
Increase case identification
With unmatched accuracy
Detect emerging issues of intentional or unintentional FWA faster
Enabling your SIU team to respond
Meet compliance mandates
Within required timeframes
Offload some or all operations
To allow SIU teams to focus on highest priority cost containment efforts
Scale SIU operations
By supplementing your current team’s efforts with virtual services
Medical record review
Experts in professional, facility, pharmacy, and dental records reviews
Use Your Limited Resources Wisely by Offloading SIU Operations to Our Expert Team
Extending your team’s FWA investigations is a great way to increase bandwidth, focus on qualified cases, and recover more of the costs lost to fraud. Codoxo’s Virtual SIU Services include:
- End-to-end SIU capabilities
Codoxo’s onshore services cover identifying and investigating possible acts of fraud, waste, or abuse, across all or any claim type, including professional, facility, dental, pharmacy, and vision - End-to-end investigative support
From initial data analysis to compliance reporting, Codoxo’s team handles the entire lifecycle to ensure thorough and efficient case management - Create & manage cases
Leverage our Fraud Scope platform to easily assign cases to our experts and securely share information and status updates - Analyzing provider service & billing patterns
Review policies and procedures to detect and identify leads - Quickly report suspect leads
Communicate to the client within required time frames
- Expert team augmentation
Access certified fraud examiners, clinical professionals, and industry specialists to scale your investigative capabilities without additional in-house hiring - Customizable reporting & compliance
Generate tailored reports to meet specific regulatory and organizational requirements, ensuring adherence to state and federal mandates - Seamless data integration
Simplify operations with expert-managed data implementation across all claim types, reducing fragmentation and enhancing clarity - Compliance reporting
Federal, state, and plan-specific reporting supported - Request & review medical/dental records
Within required time frames
Unlock Millions in Identified Exposure With Outsourced Virtual SIU Services
Smarter Healthcare Cost Containment Starts With Codoxo
Virtual SIU Services are delivered through Codoxo’s Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI and generative AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
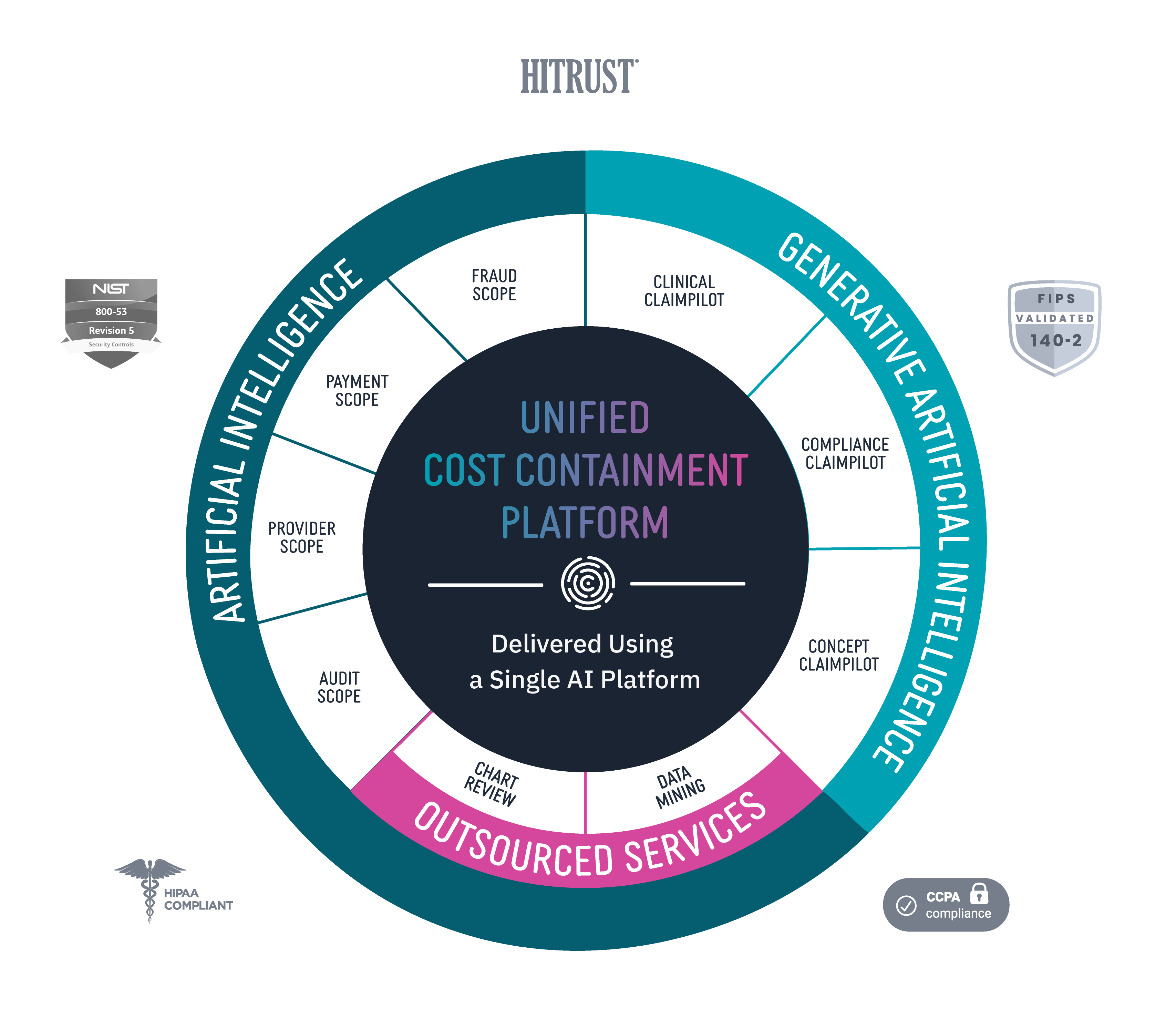
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.