Reduce the Operational Burden on Your Payment Integrity Team Through Generative AI-Driven Payment Integrity Services
Harness the potential of outsourced services to offload your team and focus on what matters most. Maximizing recoveries and achieving savings.
By offloading these tasks to Codoxo experts, your team can dedicate more time to program-driven initiatives while uncovering additional overpayments and identifying new cost-saving opportunities.
Protect Every Healthcare Dollar.
Optimize Healthcare Payments With AI-Driven Services
Codoxo offers a complete set of professional payment integrity and SIU services delivered by our team of payment integrity and fraud, waste, and abuse experts.
Our team uses the Codoxo Unified Cost Containment Platform to review your health plan’s claims data intelligence. The platform stores and analyzes data quickly, and enables our team to deliver actionable services quickly, accurately, and securely.
Customizable to your specific needs, our team can assist with a variety of functions, from data integration, data migration and data mining, to medical record and complex chart reviews, to partially or fully outsourced virtual SIU services. By outsourcing some, or all, of your payment integrity operations to Codoxo, you’ll be able to quickly augment internal resources, maximize usage and speed of our award-winning platform, and ensure claim accuracy with greater recoveries.
Explore Codoxo’s AI-Powered Outsourced Services
Free your team and maximize savings and recoveries with generative AI-driven payment integrity services:
Data Mining Services
Identify hidden opportunities for savings by uncovering outlier patterns with unmatched speed and precision.
Medical Record Reviews Services
Accelerate and optimize complex clinical reviews to drive faster recoveries and improve decision-making. Review types can include: DRG Validation, DRG Clinical Validation, Short Stay, Itemized Bill, Outpatient, and Professional claims.
Virtual SIU Services
Expand your Special Investigations Unit’s capacity with expert-led services for all or some of your SIU operations.
Achieve More with Codoxo—Your Partner in Smarter, AI & Gen AI-Powered Payment Integrity
Maximize recoveries
Uncover overpayments, billing errors, and fraud faster with AI-driven insights that identify patterns missed by traditional data mining tools
Streamline operations
Scale your SIU efforts with virtual services, enabling faster detection, investigation, and resolution of fraud, waste, and abuse
Proactively control costs
Detect and respond quickly to emerging fraud schemes and operational inefficiencies, delivering measurable ROI
Empower teams
Free internal teams from labor-intensive tasks, allowing them to focus on higher-value initiatives and strategic priorities
AI-driven precision
Go beyond rules-based methods to deliver faster, more accurate overpayment identification while minimizing errors and compliance risks
Enhance accuracy & compliance
Mitigate compliance risks with advanced generative AI technology that ensures state and payer requirements are met within mandated timeframes
Leverage generative AI
Codoxo’s team is able to gain deeper and faster insights with generative AI-enabled services that analyze data and uncover opportunities more accurately than ever before
Improve recovery outcomes
Achieve better financial results by identifying overpayments and irregularities that traditional methods often miss
Flexible, end-to-end support
Customize services to fit your organization’s needs, from anomaly detection to provider engagement and fund recovery, ensuring a seamless process from start to finish
Speed Outcomes & Efficiency With Codoxo’s Outsourced Services
97%
of overpayments captured
days to < 24 hours
reduced audit turnaround times
Removes Restrictions
$162,000
secured in recoveries from a single claim
2-3 to 20+
increased audits per day
Immediately Impacts
prepay and postpay programs
Smarter Healthcare Cost Containment
Starts With Codoxo
Codoxo’s products, services, and solutions are delivered through our Unified Cost Containment Platform, empowering healthcare organizations to take a seismic shift left by ensuring faster, more accurate claim payments, reduced healthcare fraud, waste, and abuse, and enhanced operational efficiency. By transforming the landscape of healthcare cost containment and payment integrity with industry-leading AI, Codoxo is at the forefront of making healthcare more affordable and effective.
Explore Codoxo’s Unified Cost Containment Platform
Products & Services
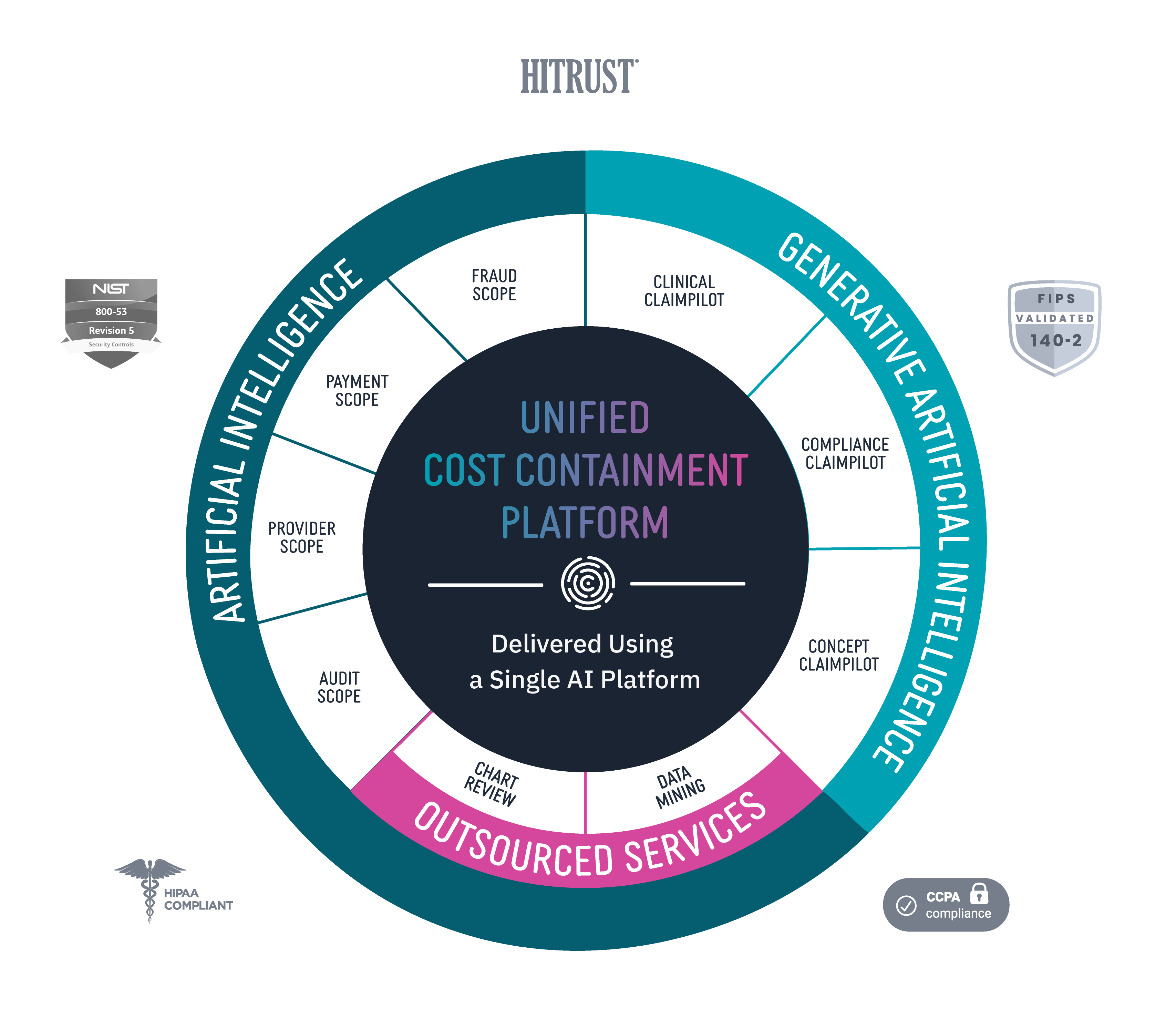
Provider Scope
Bring down costs pre-claim with proactive and automated provider education.
Audit Scope
Automate and streamline end-to-end audit detection and workflow while ensuring compliance.
Fraud Scope
Automatically and accurately detect new and emerging fraud schemes, streamline evidence chain collections, and integrate workflows for FWA investigations.
Payment Scope
Identify claim accuracy issues before claims are paid with unique claim insights, easy-to-use claim workflow, and automated provider outreach.
Clinical ClaimPilot
Automate medical record reviews with generative AI, speeding up reviews and increasing audit accuracy.
Compliance ClaimPilot
Validate provider contracts and medical policies to ensure payment accuracy and reduce manual errors.
Concept Claimpilot
Accelerate concept development of new claim payment methods and proactively spot payment gaps with generative AI.
Medical Record Reviews Services
Speed turnaround times and increase accuracy for in-patient, facility, and DRG audits with generative AI-driven medical record reviews services.
Data Mining Services
Uncover more overpayments with AI-driven outsourced healthcare data mining services.
Virtual SIU Services
Offload SIU compliance and scale operations through end-to-end virtual resources and services.