The NAMPI Virtual conference wrapped just over a week ago, and it was a great success. This conference provided ample opportunity for attendees to network, gain knowledge and capture practical insights to take back to their state agency organizations.
During the conference, Codoxo had the opportunity to share its own application of using artificial intelligence to fight fraud, waste, and abuse and contain costs. If you missed the Codoxo/Driscoll (DHP) session during the conference,
Small SIU Team Found AI-Driven Technology Met Scalability Needs, check out the recap below.
Small SIU Team Found AI-Driven Technology Met Scalability Needs
The Codoxo vendor session was co-presented by
J.R. Trevino, Manager, Special Investigations Unit at Driscoll Health Plan,
Veronica Villarreal, Investigative Analyst at Driscoll Health Plan, and
Derik Ciccarelli, Healthcare Fraud Analyst at Codoxo.
Driscoll Health Plan was founded in 1998 and is headquartered in Corpus Christi, Texas. The plan serves over 220,000 Medicaid members across the south Texas region. In 2014-2015, nine health plans in Texas sought an analytics vendor and selected a one-size-fits-all approach. During this time, Driscoll moved their SIU in-house, operating with a team of only two investigators. Due to significant growth across the plan, Driscoll sought a new analytics partner to help this small but mighty team scale operations and augment their current fraud detection services. Specifically, they looked for an analytics partner who could:
-
- Augment their SIU team domain knowledge and insights
- Deliver a comprehensive and customizable solution
- Quickly identify potential leads of FWA
- Equip them with actionable intelligence to allow for rapid identification of emerging trends and effective mitigation
After vendor analysis and evaluation, Driscoll Health Plan selected Codoxo as their partner. Codoxo was the only vendor with patented AI technology and the ability to demonstrate rapid validation of ROI. Additionally, Driscoll was drawn to Codoxo as they delivered a highly customizable and comprehensive solution.
Once the Codoxo Fraud Scope platform was implemented, Driscoll soon realized the value of having case management and case analytics in the same solution. When a suspicious trend was found, they could quickly open a case and share it with others as needed. The ability to easily validate outliers paired with their team’s deep knowledge of their providers enabled them to quickly move on leads and identify false positives. Before their partnership with Codoxo, they were operating across 3-4 different platforms. Today, they work in one.
“Before partnering with Codoxo, we were using 3-4 systems for fraud detection; now we use only one.”
– J.R. Trevino, Manager, Special Investigations Unit, Driscoll Health Plan
Driscoll has realized the value in the solution outside of the SIU as well, including the ability to share insights and access to the solution across departments, including alternative payments, provider relations, claims, medical leadership, and pharmacy. These stakeholders have access to the solution and can perform the same level of analysis as the SIU team. The easy-to-use, intuitive tool empowers cross-team collaboration regardless of experience or training.
One example provided by Driscoll is their current work with their Utilization Management (UM) department. Currently, they run reports within the tool to share with their UM team and their medical leadership. These reports showcase different trends that expose what is happening with various procedures and medications that have had a prior authorization added or removed. These reports identify usage and show where the increase and peaks exist.
During the session, Driscoll shared two use cases surrounding their use of the Codoxo AI platform to identify and quickly intervene with outlier behavior.
Use Case: Outlier Provider Billing for LARC Devices
Driscoll began receiving second authorization requests from members for Long-Acting Reversible Contraception (LARC) devices which drove them to conduct initial research surrounding the patients and providers.
The Director and Pharmacy Technician observed alarming trends, including many instances where Driscoll paid claims for a LARC device, yet no subsequent charges for the implant.
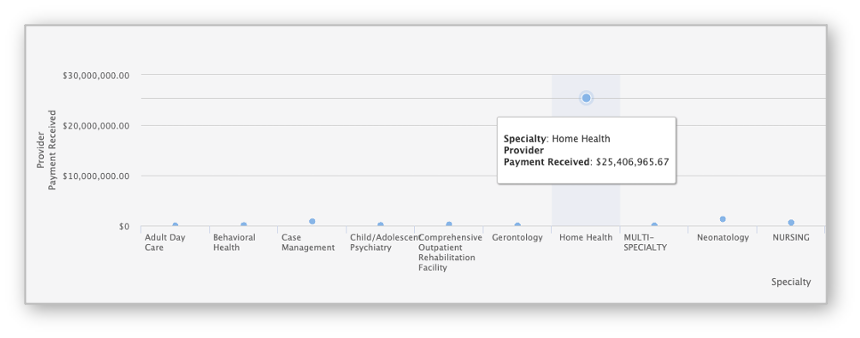
The Driscoll SIU teamed up with Codoxo to investigate. They used Codoxo’s AI-based FWA solution to analyze contraceptive implant and removal services and found anomalies in the population’s reimbursement and utilization for implants and insertions. They conducted ongoing claims and patient impact analysis while building the case using the Codoxo Case Management tool within the Fraud Scope solution.